The Affordable Care Act’s (ACA) contraceptive coverage guarantee requires most private health plans to cover the full range of contraceptive methods and services without out-of-pocket costs. However, the policy currently excludes vasectomies and male condoms. A new analysis in the Guttmacher Policy Review discusses potential pathways to rectify this serious shortcoming, including state-level actions and new recommendations from the U.S. Preventive Services Task Force (USPSTF).
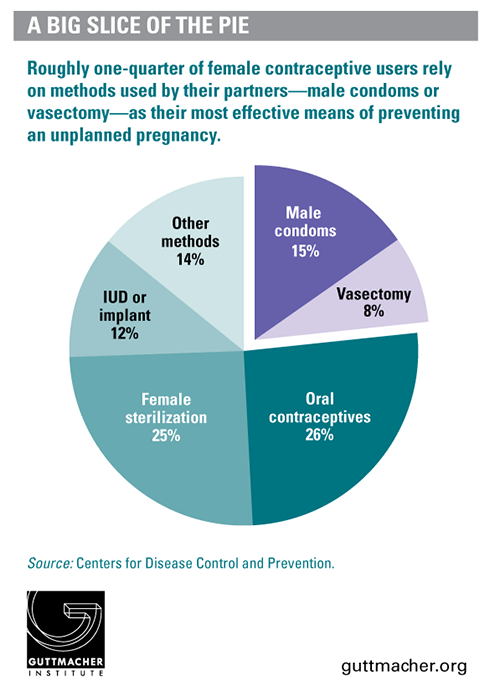
Because the section of the ACA under which the contraceptive coverage policy was established refers to preventive care "with respect to women," it has been interpreted to exclude methods that are used by men, despite strong evidence that these methods provide preventive health benefits for women by helping them prevent unplanned pregnancies and space wanted ones. The impact is considerable: 15% of women who use contraceptives rely on male condoms as their primary method and 8% rely on their partner’s vasectomy; in total, about nine million women rely on contraceptive methods used by men.
"The exclusion of methods used by men simply makes no sense and benefits no one—not men, not women, not families, not health plans," says Adam Sonfield, author of the new analysis. "Instead, it interferes with contraceptive choice and effective use. It creates a financial incentive for couples to choose female tubal ligation over less invasive and less expensive male vasectomy. And it perpetuates the all-too-common view that contraception is solely the woman’s responsibility."
Sonfield details a number of possible approaches to address this gap, including several that appear unlikely to succeed: Congress—a majority of which is hostile to the ACA as a whole—could amend the law, or the administration could reverse itself and revise its now long-standing regulations. Other approaches, even if they succeed, may be limited in their potential impact, such as individual health plans deciding on their own or under public pressure to cover these methods and exempt them from copayments and deductibles.
In a somewhat more promising approach, state policymakers could expand the ACA provision to include methods used by men. This would be a piecemeal solution, affecting only some private health plans in some states. Nevertheless, such requirements could have far-reaching ripple effects over time.
Perhaps most promising, any health care service or supply receiving a positive recommendation from the USPSTF is automatically incorporated into the ACA’s preventive services requirement—the provision that forms the basis of the contraceptive coverage guarantee. The evidence strongly supports a recommendation for contraceptive use to prevent unintended pregnancy and improve pregnancy spacing.
"Urging the U.S. Preventive Services Task Force to follow the wealth of evidence and recommend contraception as effective preventive health care has real potential to achieve coverage equity between male and female methods," says Sonfield. "It would be the right thing to do. And it would help solidify the ACA’s contraceptive coverage guarantee more generally by insulating it from political interference by future administrations."
Read the full analysis: "Rounding Out the Contraceptive Coverage Guarantee: Why ‘Male’ Contraceptive Methods Matter for Everyone," by Adam Sonfield.