- Despite large reductions in pregnancy-related deaths in Uganda over the past two decades (the maternal mortality ratio dropped from 684 per 100,000 live births in 1995 to 343 per 100,000 in 2015), the high number of maternal deaths there remains a public health challenge.[1]
- Unsafe abortion continues to contribute significantly to this public health problem: A 2010 report by the Ugandan Ministry of Health estimated that 8% of maternal deaths were due to unsafe abortion.[2]
- Ugandan law explicitly allows abortion to save a woman’s life. However, the 2006 National Policy Guidelines and Service Standards for Sexual and Reproductive Health and Rights go even further—permitting abortion under additional circumstances, including in cases of fetal anomaly, rape and incest, or if the woman is HIV-positive.[3]
- Yet, existing laws and policies on abortion are interpreted inconsistently by law enforcement and the judicial system, which makes it difficult for women and the medical community to understand when abortion is permitted.[4]
- Because of this ambiguity, medical providers are often reluctant to perform an abortion for any reason, out of fear of legal consequences.[4]
INCIDENCE OF INDUCED ABORTION
- In Uganda, an estimated 314,300 abortions took place in 2013. This translates to 14% of all pregnancies—or a rate of 39 per 1,000 women aged 15–49, down from 51 per 1,000 in 2003.
- The abortion rate for Uganda is slightly higher than the estimated rate for the East Africa region as a whole, which was 34 per 1,000 women during 2010–2014.[5]
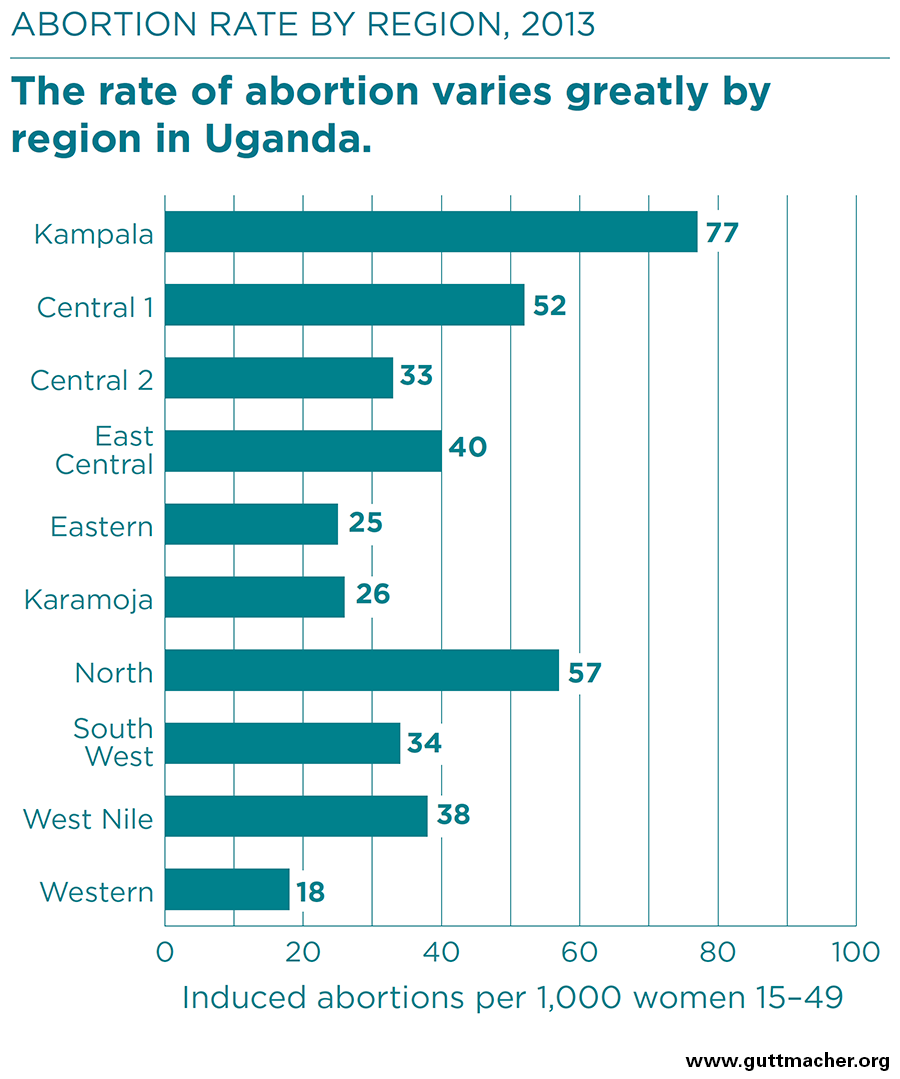
- Within Uganda, abortion rates vary widely by region, from 18 per 1,000 women in the Western region to 77 per 1,000 in Kampala.
AVAILABILITY OF POSTABORTION CARE
- Of the 2,300 health care facilities across Uganda that can provide postabortion care, an estimated 89% treat postabortion complications.
- In 2013, 93,300 women were treated for complications from unsafe abortion. This translates to an annual treatment rate for complications from unsafe abortion of 12 per 1,000 women aged 15–49, slightly down from 15 per 1,000 in 2003.
- Despite a decline in this treatment rate, injuries and illness resulting from unsafe abortion remain a critical challenge for the Ugandan health system.
HIGH COST OF ABORTION AND POSTABORTION CARE
- The amount women pay for a clandestine abortion varies. In 2011–2012, the average out-of-pocket cost for an unsafe procedure, treatment of complications prior to arriving at a health facility or both was US$23.[6] In 2003, an abortion was estimated to cost a woman US$25–88 if performed by a doctor, US$14–31 if performed by a nurse or midwife, US$12–34 if performed by a traditional healer and US$4–9 if self-induced.[7]
- The cost to the health care system of treating complications from unsafe abortion was, on average, nearly US$131 per patient in 2010.[8]
- In total, postabortion care is estimated to cost nearly US$14 million annually in Uganda. Two-thirds of this amount—US$9.5 million—is spent on nonmedical costs (overhead and infrastructure), and the remaining US$4.4 million is spent on drugs, supplies, labor, hospitalization and outpatient fees.[8]
- Most direct medical costs of postabortion care arise from treating incomplete abortion; however, a significant proportion is spent treating more serious complications, such as sepsis, shock, lacerations and perforations.[8]
IMPACT OF UNINTENDED PREGNANCY
- Most abortions are the result of unintended pregnancy. In Uganda, 52% of pregnancies are unintended, and about a quarter of these unintended pregnancies end in abortion each year.
- Between 2003 and 2013, the proportion of married women aged 15–49 using a modern contraceptive method increased from 14% to 26%; however, the proportion of unmarried sexually active women aged 15–49 using a modern method remained stagnant at 38% during this period.
- Meeting women’s contraceptive needs is a critical strategy to help women avoid unintended pregnancies. In Uganda, four out of 10 married women and almost half of sexually active women of reproductive age have an unmet need for modern contraception—that is, they want to avoid a pregnancy, but are either not practicing contraception or are using a traditional method, which can have high failure rates.
RECOMMENDATIONS
- Ensure that free or affordable public-sector family planning services reach all women—especially those who are poor and young—to reduce unmet need for contraception and lower the incidence of unintended pregnancy. Programs should offer comprehensive family planning services—including counseling and a wide range of contraceptive methods—to enable women to choose the best methods for themselves, to use methods effectively and to switch methods when desired.
- Expand and improve the quality of postabortion care services to treat the often serious health complications resulting from unsafe abortion. Health authorities should allocate greater resources to postabortion care and prioritize incorporating counseling and provision of contraceptives into this care.
- Clarify Uganda’s abortion law and policies, and raise awareness of the content and scope of Uganda’s abortion law among the medical community, the judicial system and women.