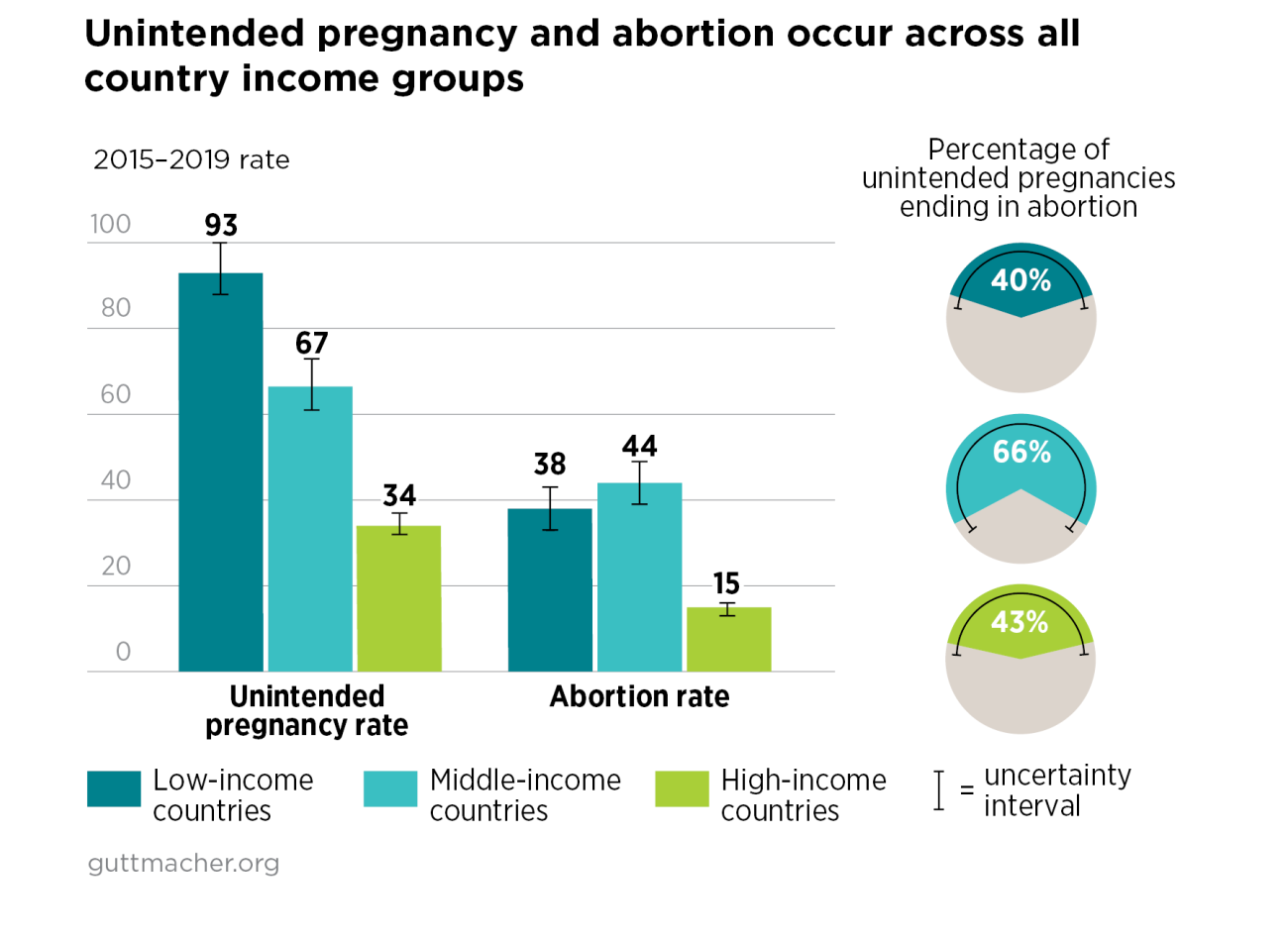
- Unintended pregnancy and abortion are experiences shared by people around the world. These reproductive health outcomes occur irrespective of country income level, region or the legal status of abortion.
- Roughly 121 million unintended pregnancies occurred each year between 2015 and 2019.*
- Of these unintended pregnancies, 61% ended in abortion. This translates to 73 million abortions per year.
Unintended Pregnancy and Abortion Worldwide
Abortion restrictions
- Abortion is sought and needed even in settings where it is restricted—that is, in countries where it is prohibited altogether or is allowed only to save the women’s life or to preserve her physical or mental health.
- Unintended pregnancy rates are highest in countries that restrict abortion access and lowest in countries where abortion is broadly legal.
- As a result, abortion rates are similar in countries where abortion is restricted and those where the procedure is broadly legal (i.e., where it is available on request or on socioeconomic grounds).
- In analyses that exclude China and India, whose large populations skew the data, the abortion rate is actually higher in countries that restrict abortion access than in those that do not.
- In countries that restrict abortion, the percentage of unintended pregnancies ending in abortion has increased during the past 30 years, from 36% in 1990–1994 to 50% in 2015–2019.

Trends in unintended pregnancy and abortion
- The global unintended pregnancy rate has declined since 1990–1994 from 79 to 64 per 1,000 women of reproductive age (15–49).
- The proportion of unintended pregnancies ending in abortion was 51% in 1990–1994, and it stayed roughly the same through 2000–2004. It then increased to 61% by 2015–2019.
- The global abortion rate decreased slightly between 1990–1994 and 2000–2004 and has since returned to levels last seen in the 1990s.

Need for a comprehensive approach
- The disparities in unintended pregnancy and abortion among low-, middle- and high-income countries indicate a need for greater action to achieve global equity in sexual and reproductive health. Continued investment is needed to ensure access to the full spectrum of high-quality sexual and reproductive health care. The Guttmacher-Lancet Commission recommends that a comprehensive package of essential sexual and reproductive health services, including contraception and safe abortion care, be included in national health systems.
- Upholding commitments to sexual and reproductive health and rights would result in better outcomes for all, and is necessary to achieve the targets set forth in numerous global goals and programs.
Source
The information in this fact sheet is based on Bearak J et al., Unintended pregnancy and abortion by income, region, and the legal status of abortion: estimates from a comprehensive model for 1990–2019, Lancet Global Health, 2020, 8(9):e1152–e1161, https://doi.org/10.1016/S2214-109X(20)30315-6. Rates and trends in this fact sheet were re-estimated using a revised data set, available on OSF.
*All rates, percentages and numbers presented in this fact sheet are annual averages for the specified five-year period. Some graphics in this fact sheet present estimates with 80% uncertainty intervals, which correspond to the 10th and 90th percentiles of the posterior distributions. These intervals signify that there is a 10% chance that the true outcome is below the interval and a 10% chance that the true outcome is above the interval. Rates represent the number of events per 1,000 women aged 15–49.
Footnotes
*All rates, percentages and numbers presented in this fact sheet are annual averages for the specified five-year period. Some graphics in this fact sheet present estimates with 80% uncertainty intervals, which correspond to the 10th and 90th percentiles of the posterior distributions. These intervals signify that there is a 10% chance that the true outcome is below the interval and a 10% chance that the true outcome is above the interval. Rates represent the number of events per 1,000 women aged 15–49.
Acknowledgments
This fact sheet was made possible by a grant from the Dutch Ministry of Foreign Affairs and by UK Aid from the UK Government. The views expressed are those of the authors and do not necessarily reflect the positions and policies of the donors.
Reproductive rights are under attack. Will you help us fight back with facts?