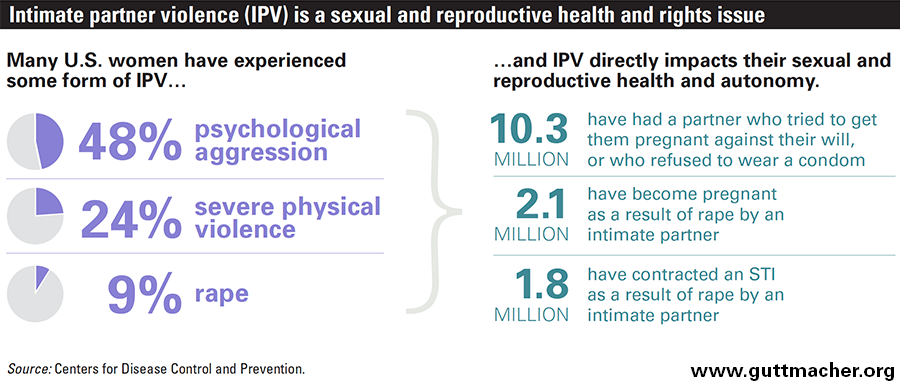
Intimate partner violence (IPV) is undeniably a public health crisis in this country—one that disproportionately affects women and has profound implications for their sexual and reproductive health and autonomy. Large proportions of U.S. women have experienced forms of violence by an intimate partner: nearly half have experienced psychological aggression, approximately one in four have been subjected to severe physical violence, and nearly one in 10 have been raped.1
Further, a third of all women who are murdered in the United States are killed by a current or former male partner.2 The most recent estimates of public costs associated with IPV exceed $8 billion annually, including more than $1 billion associated with life lost.3,4
IPV encompasses multiple forms of aggression or violence perpetrated by a current or past intimate partner, and affects people from all types of demographic backgrounds. Experiencing IPV can have a broad range of negative effects on individuals and families, including economic instability, mental health consequences and myriad physical health complications.3 Among the many issues related to IPV, there are compelling reasons to specifically examine the impact of IPV on women’s sexual and reproductive health and autonomy. In particular, certain manifestations of IPV—especially, forms of sexual violence and reproductive control—have been linked to negative sexual and reproductive health outcomes. Moreover, it is women of reproductive age—most often, those who are young or poor—who are most likely to experience IPV, including sexual violence and reproductive control.
An increasing body of evidence demonstrates the importance of understanding and addressing IPV as a critical component of sexual and reproductive health and rights (SRHR) in the United States. Toward that end, there is much to be gained if SRHR advocates and service providers were to better understand key policies and programs addressing IPV aimed at impacting health service provision.
IPV and SRHR
As defined by the Centers for Disease Control and Prevention (CDC), IPV encompasses acts of stalking, psychological aggression, physical violence or sexual violence—behaviors and tactics through which an intimate partner seeks to establish and maintain power over another. An "intimate partner" is a person to whom someone is currently or has been intimately connected, such as a spouse or domestic partner, a boyfriend or girlfriend, or a dating or ongoing sexual partner.5 (Other forms of violence, such as family violence or childhood sexual abuse, have both an immediate and a lifelong impact on those involved, but do not fall under the scope of IPV, so they are not addressed here.)
A number of negative sexual and reproductive health outcomes have been linked to IPV, but by its very nature, sexual violence in particular puts a woman experiencing it at a heightened risk for these poor outcomes. The CDC describes sexual violence as an attempted or committed sexual act perpetrated against a person who has not freely given consent or is unable to refuse.5 This includes rape, other forced or unwanted sexual contact, and unprotected sexual contact to purposefully expose an intimate partner to STIs, including HIV. Notably, the vast majority of perpetrators of rape or any other form of sexual violence against women are male.6
Related to sexual violence are acts of reproductive control. A 2010 analysis defined reproductive control as occurring when a woman’s male partner uses intimidation, threats or violence to impose his own intentions upon her reproductive autonomy—regardless of whether those intentions align with the woman’s own reproductive choices and goals.7 Reproductive control includes acts of sexual violence, contraceptive sabotage, pressuring a woman to become pregnant against her will, and coercing a woman to either carry a pregnancy to term or have an abortion.
Unintended Pregnancy and Abortion
U.S. women who are most at-risk of experiencing IPV are also likely to have a particularly high risk of experiencing an unintended pregnancy. Indeed, IPV is most prevalent among women of reproductive age.1 More specifically, the unintended pregnancy rate in the United States is highest among women aged 18–24, the age group with the highest prevalence of IPV.1,8
The risk of unintended pregnancy is especially salient for women experiencing male reproductive control or sexual violence. Behaviors such as birth control sabotage or pregnancy pressure directly impede a woman’s ability to properly use her preferred method of contraception and compromise her ability to avoid a pregnancy she does not want. Indeed, women who are not consistently and correctly using a contraceptive method account for 95% of unintended pregnancies in the United States;9 this includes women who are unable to use contraception consistently and correctly because of reproductive control or sexual violence.7 According to the 2010 National Intimate Partner and Sexual Violence Survey, an estimated two million women in the United States have ever become pregnant as a result of rape by an intimate partner (see chart).6 Five percent of women reported that, at some point in their lifetime, an intimate partner had tried to impregnate them when they did not want to get pregnant.1
Even though abortion rates specific to women who experience an unintended pregnancy resulting from IPV are unknown, many women may be highly motivated to terminate these pregnancies. (Among all women, about four in 10 unintended pregnancies in the United States end in abortion.8) According to a nationally representative Guttmacher Institute study of women obtaining abortions from hospitals, clinics and physicians’ offices in the United States, 7% reported having experienced IPV by the man involved in the pregnancy.10 The same study also found that women who had experienced IPV were significantly less likely than others to report that the man involved in the pregnancy knew about or was supportive of the abortion. This complements previous findings linking IPV to women’s decisions not to disclose their abortions; women with histories of abuse or who fear physical harm are much less likely to involve men in their decision to obtain an abortion.
Additionally, other evidence suggests that male reproductive control may manifest as pressure to terminate a pregnancy when the woman does not want to do so.7 And further research has found a link between women seeking repeat abortions and having been subjected to physical or sexual violence.11
Poor Maternal and Infant Health Outcomes
IPV has a negative impact on the health of pregnant and postpartum women and their infants. This is especially true when a woman’s partner physically harms her while she is pregnant—in some cases with the intent to cause a miscarriage. One analysis of CDC data found that nearly 4% of pregnant women reported being physically abused by a current or former partner during pregnancy and that the strongest predictor of physical violence was if the partner did not want the pregnancy.12
IPV among women prior to or during a pregnancy has also been linked to many pregnancy complications.13,14 For instance, women experiencing IPV are at greater risk for rapid, repeat pregnancies, potentially limiting the demonstrated health benefits of planning and spacing pregnancies.7,15 And women experiencing IPV before becoming or while pregnant are less likely to obtain early prenatal care, and are more likely to experience preterm labor and have low-birth-weight infants.13,15,16 One study found that having experienced IPV before delivery was associated with four times the odds of stillbirth;14 other studies have found a link between IPV and postpartum depression.17,18
HIV and Other STIs
An estimated 1.8 million U.S. women have contracted an STI as a result of rape by an intimate partner at some point in their lives.6 And sexual violence is not the only form of IPV that can increase women’s risk of STIs; male reproductive control behaviors include refusing to use condoms, and women experiencing IPV may be or perceive themselves to be unable to negotiate condom use or monogamy.7
Indeed, multiple reviews of available evidence have documented associations between lifetime experience of IPV and lifetime acquisition of an STI.19–21 Experiencing IPV has also been associated with a woman’s increased likelihood of engaging in risky reproductive and sexual behaviors—such as having multiple concurrent sexual partners and using condoms inconsistently—that can contribute to a heightened risk for STIs.22–24
Untreated STIs can lead to additional negative sexual and reproductive health outcomes, including pelvic inflammatory disease, infertility, cancer and possible pregnancy complications.25–27 Women experiencing IPV may be less likely to obtain care for HIV or other STIs, given that an abusive partner may also deny her access to health care as another way to exert control. And IPV can lead to particularly detrimental health outcomes for women living with HIV.28
Notably, one review of evidence concluded that although similar proportions of HIV-positive women and HIV-negative women experience IPV in the United States, those living with HIV experience a greater number and more violent instances of IPV.29 This is particularly concerning because the negative health outcomes of IPV may compound according to the frequency, severity or duration of violent exposures.19
Federal Policies Addressing IPV
Given the existing and expanding body of evidence that IPV is inextricably tied to sexual and reproductive health and autonomy, understanding where these two issue areas intersect at the federal policy level is critical to better addressing the needs of those experiencing IPV and to better supporting safety-net providers in doing so.
The bulk of federal policy and funding intended to address IPV in the United States is directed to legal and criminal justice interventions, or to funding for victim services; yet, an increasing amount of attention is being paid to violence prevention. Three major policy initiatives form the core of the national response to violence and sexual assault: the Family Violence Prevention & Services Act (FVPSA), the Victims of Crime Act (VOCA) and the Violence Against Women Act (VAWA). Agencies within the Department of Health and Human Services (DHHS) and the Department of Justice (DOJ) are responsible for implementing these programs. Further, in approaching IPV as a matter of public health, both the Affordable Care Act (ACA) and the nation’s publicly supported family planning effort explicitly and directly address the health care needs of women experiencing IPV.
Family Violence Prevention & Services Act
FVPSA was initially authorized in 1984 as the first federal policy and funding stream to address IPV in the United States, and it remains the main federal source of support for direct services and assistance to IPV survivors and their families. The statute requires that DHHS grant 70% of all FVPSA funds to states and territories according to their population size. These "formula grants" support efforts to shelter survivors and their dependents, coordinate state and local administrators and coalitions, offer technical assistance and training, and raise public awareness. FVPSA also funds the National Domestic Violence Hotline and a number of national resource centers.
For FY 2016, Congress appropriated $150 million for the FVPSA programming from which formula grants are made.30 Grantees include states, territories and tribes, and state domestic violence coalitions, many of which then allocate funding to local outreach programs and shelters. Notably, 70% of an individual state’s FVPSA formula grant must go toward sheltering survivors and families, and related programming and services; although medical advocacy—including referrals—is considered a "related service," FVPSA funds cannot reimburse the provision of any actual health services. Program requirements for reaching out to underserved populations and connecting individuals experiencing IPV to services mandate collaboration with community-based organizations, which could and should extend to safety-net family planning centers.
Victims of Crime Act
In 1984 (the same year FVPSA was first authorized), VOCA established the Crime Victims Fund (CVF). This fund is made up of money from criminal fines, special assessments and bond forfeitures collected from convicted federal offenders (including but not limited to perpetrators of IPV), and is administered by the Office for Victims of Crime within DOJ.
Two types of formula grants distributed to states and territories account for the vast majority of CVF funds distributed each year. The first goes toward reimbursing crime survivors for various out-of-pocket costs related to the crime when other compensation, including private insurance, will not cover their expenses. Medical and dental care accounted for more than half of the total $424.6 million in payments made in FY 2012, followed by mental health care, economic support, and funeral and burial expenses.31 Sexual and reproductive health services are a critical component of routine medical care, and are services that women experiencing IPV are particularly likely to need. Plus, many of these women are uninsured or may be unable to use their coverage because of confidentiality concerns, which makes VOCA reimbursements an important option to defray the cost of care.
The second type of CVF formula grant supplements state funds to assist survivors in obtaining needed services and support, such as crisis intervention, counseling and referrals, advocacy throughout the criminal justice process and emergency transportation. States distribute CVF funds to subgrantees such as shelters, rape crisis centers, hospitals and social service agencies, which provide direct assistance and services. In FY 2012, 3.5 million individuals—including 1.7 million survivors of domestic violence (a term often interchanged with IPV, particularly by government entities, but which can have a more limited connotation)—benefited
from more than 5,000 subgrants.32 Safety-net family planning centers are particularly well-positioned to serve women experiencing IPV, which makes them natural—and important—participants in this grant program.
Violence Against Women Act
Understanding where IPV and sexual and reproductive health policy intersect is critical to better addressing the needs of those experiencing IPV.
First enacted in 1994 and most recently reauthorized in 2013, VAWA is often recognized as the keystone federal policy addressing violence against women in the United States. It focuses on law enforcement and legal responses to violence, and emphasizes the importance of a coordinated community response and the inclusion of myriad stakeholders—including health care professionals—in developing local support systems. Dozens of individual programs exist under the VAWA umbrella, most of which are administered by the Office on Violence Against Women within DOJ, and some by the CDC within DHHS. Some of these programs have the potential to impact the sexual and reproductive health of people experiencing IPV, as VAWA currently does address some of the health service needs of sexual assault survivors through a few of its funding streams. Health care is not generally a focus of VAWA, however, and efforts to address survivors’ health needs have thus far been largely deprioritized and underfunded.
For instance, a program called Grants to Strengthen the Healthcare System’s Response to Domestic Violence, Sexual Assault and Stalking was established in 2013 as a consolidation of three previously separate (and never-funded) efforts to bolster the public health response within VAWA. That year, VAWA authorized $10 million in annual funding for the program, which was supposed to be administered by the CDC and distribute grants to state-level partners to advance policymaking and research on effective violence interventions in health settings. However, the first hint of funding under this program did not come until FY 2015, when Congress appropriated $3.1 million to the Office on Women’s Health within DHHS to fund health programs and support providers in the states under an effort called the Violence Against Women Health Initiative. Advocates in the IPV community see this federal effort and the state partnerships it has supported among IPV and health care experts and services providers as a promising first step, and have called for additional funding and time for effective, nationwide implementation.
A number of other VAWA initiatives do not address health as directly, but could play a role in advancing access to sexual and reproductive health care for individuals experiencing IPV. These range from the Rape Prevention and Education Program; to an effort designed to reduce IPV on university campuses; to the Services, Training, Officers and Prosecutors (STOP) initiative—the largest individual VAWA program, which supports coordinated community responses to violence and identifies health care professionals as key players in the planning and implementation of state plans.
Since its inception, VAWA has included provisions to help reduce the risk of STIs for those who have been sexually assaulted, and its 2013 reauthorization included additional supports to advance access to HIV testing, counseling and prophylaxis. Yet, other health needs related to sexual assault remain unaddressed, especially those related to unintended pregnancy. Some reproductive rights advocates criticized VAWA’s 2013 reauthorizing legislation specifically for not including provisions to help women access emergency contraception in a timely manner; the reauthorization also left other pregnancy-related services, including abortion, wholly unaddressed. It did, however, make strides to prevent and respond to sexual assault on college campuses, as well as include new protections for LGBT individuals, among other disadvantaged groups.
Affordable Care Act
For women experiencing IPV, the ability to access affordable and confidential health care can be both particularly difficult and particularly important—difficult in that an abusive partner may purposefully prevent her from accessing health care, and important in that without coverage to defray the cost, women are much more likely to go without the care they need. To this end, the ACA’s coverage expansions include provisions to help ensure that individuals experiencing IPV are able to obtain affordable health insurance coverage.
To benefit from coverage, women must first obtain it. Some women and children will be eligible for enrollment in Medicaid or the Children’s Health Insurance Program, and enrollment in those programs can occur at any time throughout the year. By contrast, qualifying individuals and families can purchase coverage through the ACA’s marketplaces only during specified open enrollment periods, but the ACA established a special enrollment period for individuals experiencing domestic violence and their dependents. In states that use the federally run online marketplace, HealthCare.gov, survivors can apply for this 60-day special enrollment period at any time via phone by attesting to the fact that they are experiencing violence; no documentation is necessary. Furthermore, if a woman has moved out or been abandoned by her spouse but remains legally married and will file taxes separately from her spouse, the ACA enables that individual to lawfully check "unmarried" on her application for marketplace coverage so she can report only her individual income (rather than joint income) in determining eligibility for subsidies to make marketplace coverage more affordable.
The ACA also guarantees that individuals newly eligible for Medicaid and enrollees in most private health plans receive coverage without cost-sharing for the full range of contraceptive methods and counseling. A woman’s ability to obtain the method of contraception that will work best for her particular circumstances can be crucial for a woman seeking to avoid a pregnancy while, or because, she is experiencing or fears IPV—especially in instances of contraceptive or pregnancy coercion. A woman who discloses abuse to a family planning provider may well require extensive counseling and discussion with her clinician, and potentially a contraceptive method that could go undetected by a partner.
The ACA’s preventive health services provision also requires that screening and brief counseling for IPV be covered and provided without cost-sharing; more robust, regular counseling related to IPV may be covered under the terms of a plan’s mental health benefits. Screening and counseling may also be covered without cost-sharing under Medicaid, which may include coverage of additional related services.
Notably, health care providers are mandatory reporters and must comply with state reporting laws.33 Reporting requirements—particularly of sexual assault—vary by state, which requires family planning providers to fully understand their states’ policies and be aware of how the law might affect how they deliver care to individuals experiencing IPV.
Title X National Family Planning Program
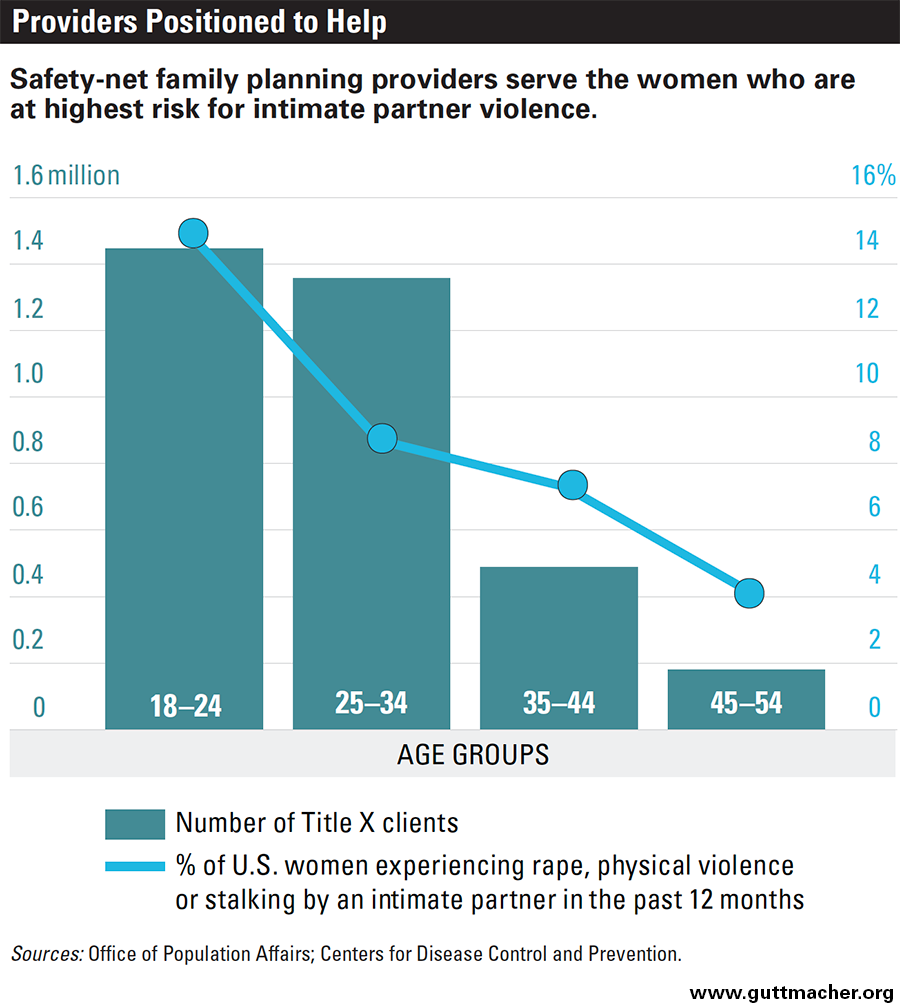
For IPV survivors, confidentiality can be a necessary condition of their obtaining needed health care services, particularly sexual and reproductive health care. Federal family planning policy has long stressed the importance of confidential care; under Title X program requirements, any health center receiving Title X funding must ensure confidentiality for all of their family planning clients, regardless of age, income or insurance status.34 These protections are particularly important given the sensitive nature of sexual and reproductive health services supported by Title X grants, and they are intended to protect the privacy of especially vulnerable groups of safety-net family planning clients. This includes women experiencing or threatened by IPV, who could suffer harm if the fact that they obtained health care services were disclosed to their partners. In fact, there is considerable overlap between groups of U.S. women at highest risk for experiencing IPV and those seeking care from Title X–supported providers (see chart).1,35
Additionally, in 2014, the U.S. Office of Population Affairs, the agency that administers the Title X program, in conjunction with the CDC, released Providing Quality Family Planning Services, a set of clinical recommendations that defines the core services of family planning care and details how that care should be delivered.36 The recommendations—which are applicable to all family planning providers, regardless of whether they receive Title X funds, or are otherwise publicly or privately funded—reiterate that client confidentiality is paramount for all individuals obtaining family planning care, especially for those experiencing IPV, and also suggest that all women of reproductive age be screened for IPV. In addition, they recommend that individuals experiencing violence be referred for further counseling, care and intervention services, and highlight the need for service providers to consider clients’ past and current experiences with IPV and other forms of violence—particularly sexual violence—when helping them choose a contraceptive method.
An Integrated Approach
IPV—especially forms of sexual violence and male reproductive control—increases women’s risk for multiple negative sexual and reproductive health outcomes. Therefore, women experiencing IPV often have an acute need for the full range of sexual and reproductive health services, including contraceptive supplies and counseling, STI testing and treatment, maternity care and abortion. This range of care must be accessible, confidential and affordable.
Notably, the ACA has advanced coverage of and access to care—particularly, preventive family planning and pregnancy-related services—for privately insured women, and women with Medicaid coverage have similarly robust benefits. For abortion coverage, the situation is more complex. The Hyde Amendment blocks federal Medicaid funds from being used to cover abortion in all but the most limited circumstances, and half the states bar abortion coverage in at least some private health plans. However, the Hyde Amendment and many of the state restrictions on private insurance do provide exceptions for cases of rape and incest (as well as cases when the women’s life is endangered by the pregnancy), which makes this coverage of potential use for some women experiencing IPV.
For all types of services, providers are increasingly recognizing the importance of providing care in a way that takes into account the many considerations—health or otherwise—that arise when a patient is experiencing IPV or another form of trauma, an approach called "trauma-informed care."37 This can include helping a woman to protect her sexual and reproductive health and autonomy in a way that also takes her safety into account, ensuring her care remains confidential and connecting her to resources that can help her address broader needs.
Achieving this type of approach to caring for those experiencing IPV requires collaboration on many levels among IPV and SRHR service providers, policy experts and advocates. For instance, safety-net family planning providers are positioned to confidentially meet survivors’ particular family planning needs and to connect them to broader resources, especially if they have received appropriate training and have mutual referral relationships with IPV experts in their communities. Indeed, a considerable body of ongoing work at the service delivery level seeks to understand how family planning providers can most effectively discern and address the particular needs of women experiencing IPV, specifically reproductive control.38 And future updates of the policies and program guidelines directing the nation’s response to IPV and the provision of quality family planning care will offer opportunities to identify and incorporate systemic changes that more inclusively address the sexual and reproductive health and autonomy of women experiencing IPV.
The barriers to effective collaboration are real. For instance, the increasingly intense and negative politics of abortion that now pervade almost anything and everything related to health care create a disincentive for many in the IPV community to overtly make the natural policy connections between IPV and SRHR. Conversely, advocates focused on SRHR may lack an understanding of IPV policy, and safety-net family planning providers may feel they lack sufficient guidance, support or experience to fully engage with a client on her experiences with IPV. There is no doubt, however, that overcoming these barriers is imperative to being able to holistically serve individuals experiencing IPV, including addressing their need for sexual and reproductive health care.