• Tanzania ni kati ya nchi zenye uwiano wa juu wa vifo vya wajawazito duniani (410 kwa kila watoto 100,000 wanaozaliwa wakiwa hai), na utoaji mimba usio salama ni moja kati ya sababu zinazoongoza.
• Utoaji mimba usio salama unachangia zaidi ya theluthi moja ya wanaolazwa mahospitalini kutokana na matatizo yanayohusiana na mimba1 na takribani robo moja ya vifo vya uzazi.2,3
• Sheria na sera ya utoaji mimba nchini Tanzania ina utata na inachanganya. Sheria ya makosa ya jinai huidhinisha utoaji mimba ili kuokoa maisha ya mwanamke, lakini haijaweka wazi kama utaratibu huu utalinda afya ya mwili na akili ya mwanamke.4 Hofu ya kushtakiwa, ambayo ipo kwa wanawake na watoa huduma ya afya pia, husababisha wanawake watoe mimba kwa siri kwa njia ambazo mara nyingi huwa si salama.
MATUKIO YA UTOAJI MIMBA
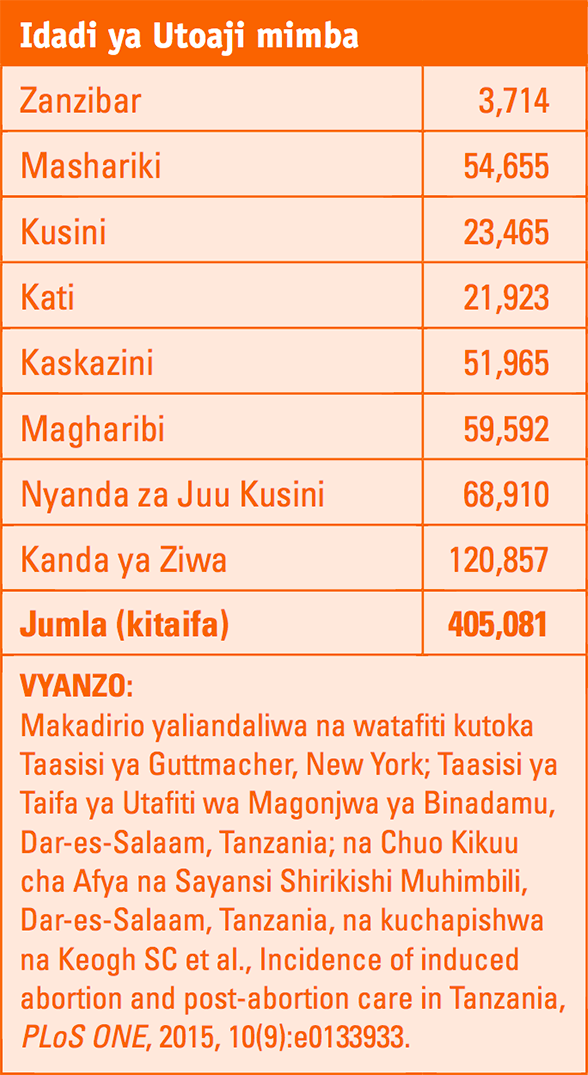
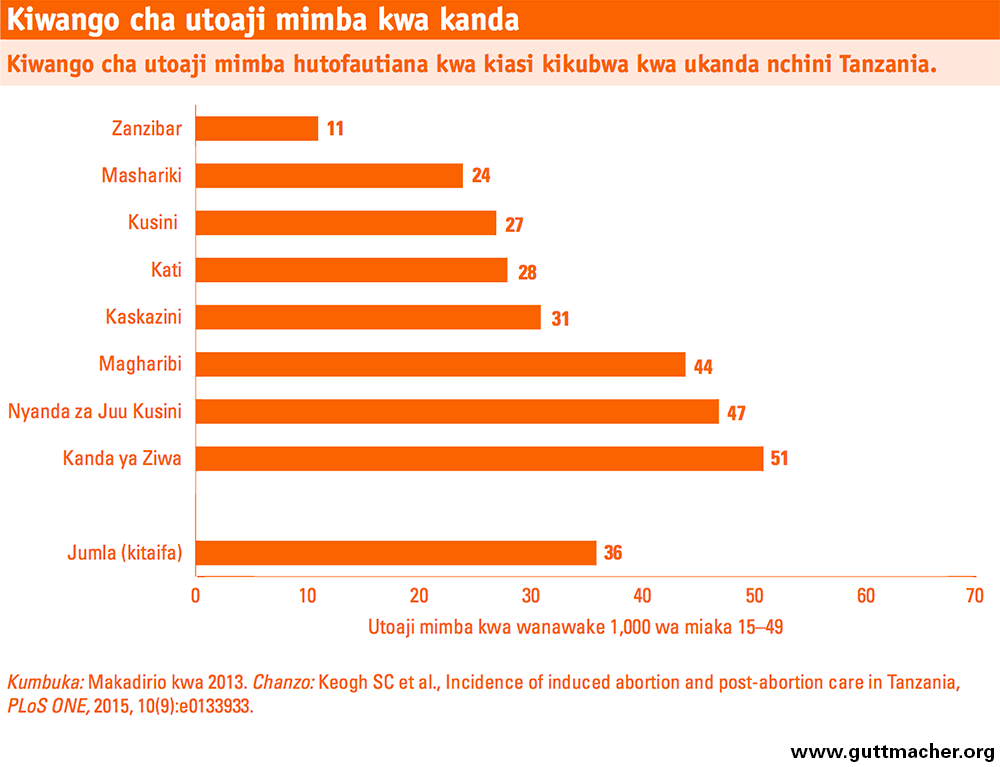
• Inakadiriwa kuwa, mimba 405,000 zilitolewa ndani ya mwaka 2013 nchini Tanzania. Idadi hii ni kiwango cha utoaji wa mimba 36 kwa kila wanawake 1,000 wenye umri kati ya miaka 15-49 na uwiano wa utoaji mimba 21 kwa kila watoto 100 wanaozaliwa wakiwa hai.
• Kiwango cha utoaji mimba ni sawa na wastani wa kiwango cha kanda ya Afrika Mashariki kwa ujumla (36 kwa kila wanawake 1,000) na juu kidogo kuliko kiwango cha nchi za Kusini mwa Sahara (31).5
• Nchini Tanzania, viwango vya utoaji mimba hutofautiana sana kwa ukanda, kutoka 11 kwa wanawake 1,000 kwa Zanzibar hadi 47 kwa Nyanda za Juu Kusini na 51 kwa Kanda ya Ziwa. Ukanda wa Ziwa na Nyanda za Juu Kusini huwa na viwango vya juu vya matibabu kwa matatizo yatokanayo na utoaji mimba pia.
• Mwaka 2013, katika nchi nzima, 15% ya mimba zilitolewa, 52% katika uzazi uliokusudiwa, 18% katika uzazi usiokusudiwa na 15% katika mimba zilizoharibika. Mgawanyo huu hutofautiana kwa maeneo kwa mfano, uwiano wa mimba zilizotolewa ni kati ya 6% kwa Zanzibar hadi 18% kwa Nyanda za Juu Kusini.
SABABU ZA VIWANGO HIVI VYA UTOAJI MIMBA
• Sababu kadhaa kueleza tofauti katika viwango vya utoaji mimba kwa ukanda: tofauti katika idadi ya watoto ambayo wanawake wanataka kuwa nao, tofauti katika tendo la kujamiiana na matumizi ya uzazi wa mpango, na tofauti katika uwezekano wa wanawake wa kutegemea utoaji mimba katika tukio la mimba zisizotarajiwa.
• Takribani mwanamke mmoja kati ya watano wenye umri kati ya miaka 15–49 nchini Tanzania wanataka kuchelewesha au kusitisha kuwa na watoto lakini hawatumii njia yoyote ya uzazi wa mpango. Kundi hili la wanawake huchukuliwa kama lenye mahitaji yasiyofikiwa ya uzazi wa mpango.
• Katika Ukanda wa Ziwa, matumizi ya chini ya uzazi wa mpango (ya chini kabisa kwa nchi nzima) na ukubwa wa mahitaji yasiyofikiwa huchangia kiwango kikubwa cha utoaji mimba na mimba zisizotarajiwa, ambacho ni cha juu zaidi nchini.
• Wanawake wenye mimba zisizotarajiwa katika Nyanda za Juu Kusini, ambapo matumizi ya uzazi wa mpango ni ya juu, wana uwezekano zaidi wa kuamua kutoa mimba kuliko wale wa maeneo mengine, na kusababisha viwango vya juu vya utoaji mimba: 59% ya mimba zisizotarajiwa ziliishia kwenye kutolewa katika Nyanda za Juu Kusini mwaka 2013, ikilinganishwa na chini ya 45% katika maeneo mengine.
• Kiwango cha chini cha utoaji mimba kwa Zanzibar, cha 11 kwa kila wanawake 1,000 wenye umri kati ya miaka 15–49, ni kutokana na kuwa na kiwango cha chini zaidi cha mimba zisizotarajiwa nchini. Ikilinganishwa na wenzao wa Tanzania bara, wanawake visiwani Zanzibar huanza vitendo vya ngono wakiwa na umri mkubwa, na walioolewa huripoti kiwango kidogo cha shughuli za ngono.
UPATIKANAJI WA HUDUMA BAADA YA KUHARIBIKA KWA MIMBA
• Karibia wanawake 67,000 walitibiwa katika vituo vya afya kwa ajili ya matatizo yanayotokana na utoaji mimba usio salama kwa mwaka 2013 nchini Tanzania. Hata hivyo, karibu wanawake wengine 100,000 ambao walipata matatizo yaliyohitaji tiba katika kituo cha afya hawakupata matibabu waliyohitaji.
• Hospitali za rufaa na mikoa hutibu wagonjwa wengi wanaopata huduma baada ya kuharibika kwa mimba; kwa wastani, kila moja ilitibu karibia wagonjwa 1,140 na 710 kwa mtiririko ndani ya mwaka 2013.
• Kwa wastani, chini ya vituo vya afya nane hutoa huduma baada ya kuharibika kwa mimba kwa kila wanawake 100,000 nchini Tanzania. Zanzibar inatoa huduma zaidi, ikiwa na vituo zaidi ya 10 kwa wanawake 100,000, wakati Ukanda wa mashariki una vituo vichache vya huduma hii—chini ya vituo sita kwa kila wanawake 100,000.
• Viwango vya tiba kwa matatizo yatokanayo na kuharibika na utoaji mimba hutofautiana kwa kiasi kikubwa na kanda, hii ni kwa sababu ya usambazwaji usiokuwa wa usawa wa watoa huduma baada ya kuharibika kwa mimba.
UIMARISHAJI WA HUDUMA BAADA YA KUHARIBIKA KWA MIMBA, NA UZAZI WA MPANGO
• Kupunguza utoaji mimba usio salama na vifo vya wajawazito na majeraha yanayohusishwa na utoaji mimba, utahitaji kupanua upatikanaji wa huduma za uzazi wa mpango ili kuzuia mimba zisizotarajiwa, na kupanua upatikanaji wa huduma za baada ya kuharibika kwa mimba.
• Vituo vya afya katika ngazi zote lazima viwe na dawa muhimu za kutosha, vifaa vya kutolea huduma za msingi za baada ya kuharibika kwa mimba, na watoa huduma wa kawaida wanapaswa wapewe mafunzo ya kutoa huduma hizo.
• Huduma baada ya kuharibika kwa mimba zitolewe sambamba ba huduma za uzazi wa mpango kwa sababu wagonjwa wanaopokea huduma baada ya kuharibika kwa mimba hupokea sana ushauri nasaha juu ya uzazi wa mpango.6,7 Tafiti zimegundua kwamba idadi kubwa ya wagonjwa hao hukubali njia za uzazi wa mpango na kuendelea kuzitumia.8
• Huduma baada ya kuharibika kwa mimba kutoa fursa ya kushirikisha wanaume katika uzazi wa mpango: Imeonekana kuwa wanaume wanaokwenda na wapenzi wao kwenye huduma baada ya kuharibika kwa mimba hupokea na taarifa za uzazi wa mpango pia.9
• Kuweka kipaumbele kwenye kanda ambazo zina viwango vya juu vya utoaji mimba, kama Kanda ya Ziwa na Nyanda za Juu Kusini, itakuwa ni njia ya gharama nafuu ya kupunguza vifo vya wajawazito na maradhi nchini Tanzania.
• Utata kuhusu sheria ya utoaji mimba ya Tanzania unatakiwa ufafanuliwe ili kusaidia kuunga mkono taratibu salama na kisheria zitumike kikamilifu, na kuhakikisha kuwa wanawake hawana sababu ya kuamua kutumia njia zisizo salama kutoa mimba zao.