Incidence and trends
- During 2010–2014, an estimated 6.5 million induced abortions occurred each year in Latin America and the Caribbean—up from 4.4 million during 1990–1994.
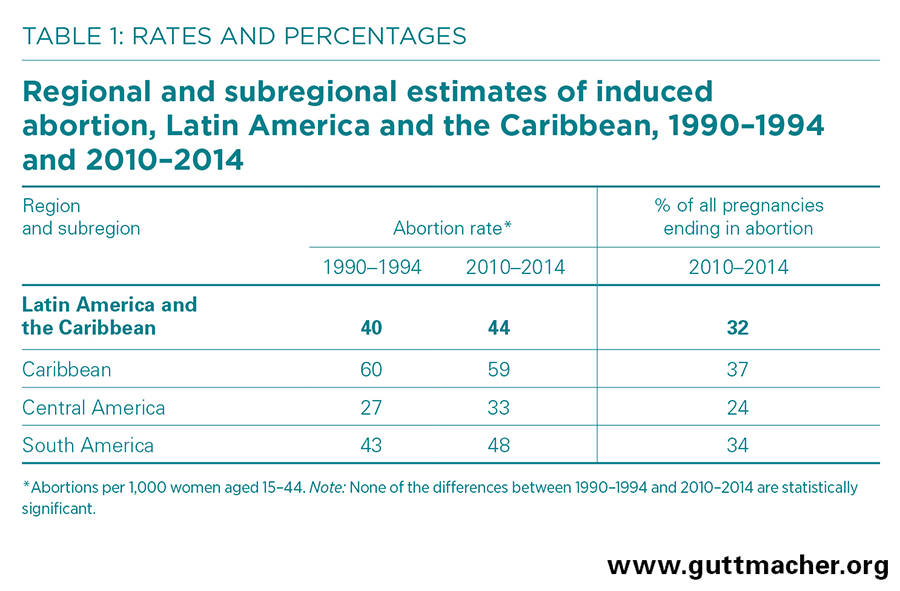
- The annual rate of abortion is estimated at 44 per 1,000 women of reproductive age (15–44), a slight increase from 40 per 1,000 in 1990–1994.
- The regional abortion rate is roughly 48 per 1,000 for married women and 29 per 1,000 for unmarried women.1
- As of 2010–2014, abortion rates range across subregions, from 33 per 1,000 women in Central America to 48 per 1,000 in South America to 59 per 1,000 in the Caribbean.
- The proportion of all pregnancies in Latin America and the Caribbean ending in abortion increased between 1990–1994 and 2010–2014, from 23% to 32%.1
Legal status of abortion
- More than 97% of women of reproductive age in Latin America and the Caribbean live in countries with restrictive abortion laws (i.e., countries in the first four categories in Table 2).2
- Abortion is not permitted for any reason in six countries. Nine others allow it almost exclusively to save the woman’s life, with only some offering limited exceptions for rape (Brazil, Chile, Mexico and Panama) and grave fetal anomaly (Chile, Panama and almost half of the states of Mexico).
- Fewer than 3% of the region’s women live in countries where abortion is broadly legal—that is, permitted either without restriction as to reason or on socioeconomic grounds.2
Unsafe abortion and its consequences
- Induced abortion is medically safe when WHO-recommended methods are used by trained persons, less safe when only one of those two criteria is met, and least safe when neither is met. Many women undergo unsafe (i.e., less safe or least safe) procedures that put their well-being at risk.
- During 2010–2014, about one in four abortions in Latin America and the Caribbean were safe. The majority (60%) of procedures fell into the less-safe category.
- About 760,000 women in the region are treated annually for complications from unsafe abortion.3
- In 2014, at least 10% of all maternal deaths (or 900 deaths) in Latin America and the Caribbean were from unsafe abortion.4
- The most common complications from unsafe abortion are incomplete abortion, excessive blood loss and infection.
- Poor and rural women are the most likely to experience an unsafe abortion and severe complications thereof.
- Postabortion services in the region are often of poor quality. Common shortcomings include delays in treatment, use of inappropriate interventions, inadequate access, and judgmental attitudes among clinic and hospital staff. These factors likely deter some women from obtaining needed treatment.
- The use of misoprostol to induce abortions is growing more common throughout the region and seems to have increased the safety of clandestine procedures.
- From 2005 to 2012, the treatment rate of complications from unsafe abortion fell by one-third, from 7.7 to 5.3 cases per 1,000 women of reproductive age. This likely represents a real decrease in complications requiring care.
Unintended pregnancy and unmet need
- As of 2017, more than 24 million women of reproductive age in Latin America and the Caribbean have an unmet need for modern contraception—that is, they want to avoid a pregnancy but are either not practicing contraception or are using traditional methods, which are less effective than modern methods.5
- Most women who have an abortion do so because they become pregnant when they do not intend to. As of 2010–2014, Latin America and the Caribbean has the highest rate of unintended pregnancy of any world region—96 per 1,000 women aged 15–44. In the subregion of the Caribbean, the rate was 116 unintended pregnancies per 1,000 women.
- An estimated 14 million unintended pregnancies occur each year in Latin America and the Caribbean; of these, nearly half (46%) end in abortion.
Recommendations
- Programs and policies that improve women’s and men’s knowledge of, access to and use of contraceptive methods must be implemented to reduce unintended pregnancies—and the abortions or unplanned births that often follow.
- The provision and quality of postabortion care should be improved and expanded to reduce illness and death from unsafe abortion.
- The grounds for legal abortion should be broadened and access to safe abortion services improved to reduce the number of clandestine procedures and the negative consequences that often result.
- Access to family planning and postabortion care should be prioritized for poor and rural women, who experience disproportionately high rates of illness and death from unsafe abortion.