Adding It Up is a research initiative that examines the need for, impact of and costs associated with fully investing in sexual and reproductive health (SRH) care in low- and middle-income countries (LMICs) around the world. These services enable individuals to make informed decisions about whether and when to have children, experience safe pregnancy and delivery, support the health of their newborns, and maintain their sexual and reproductive well-being.
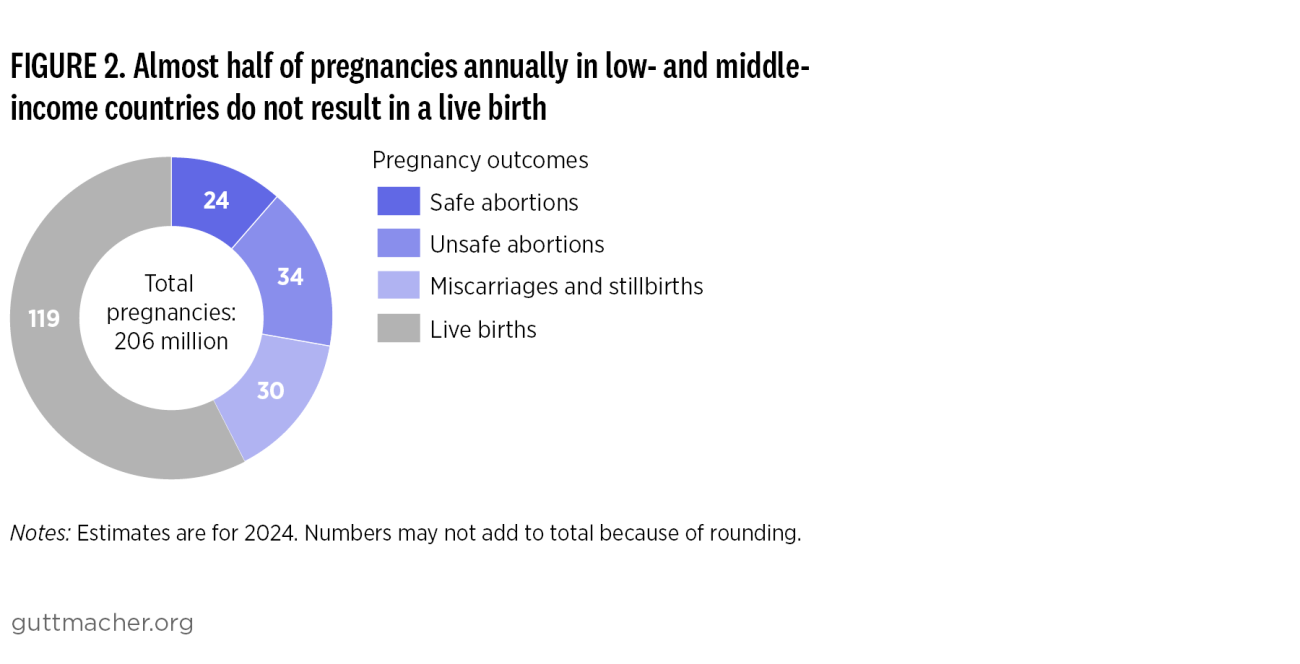
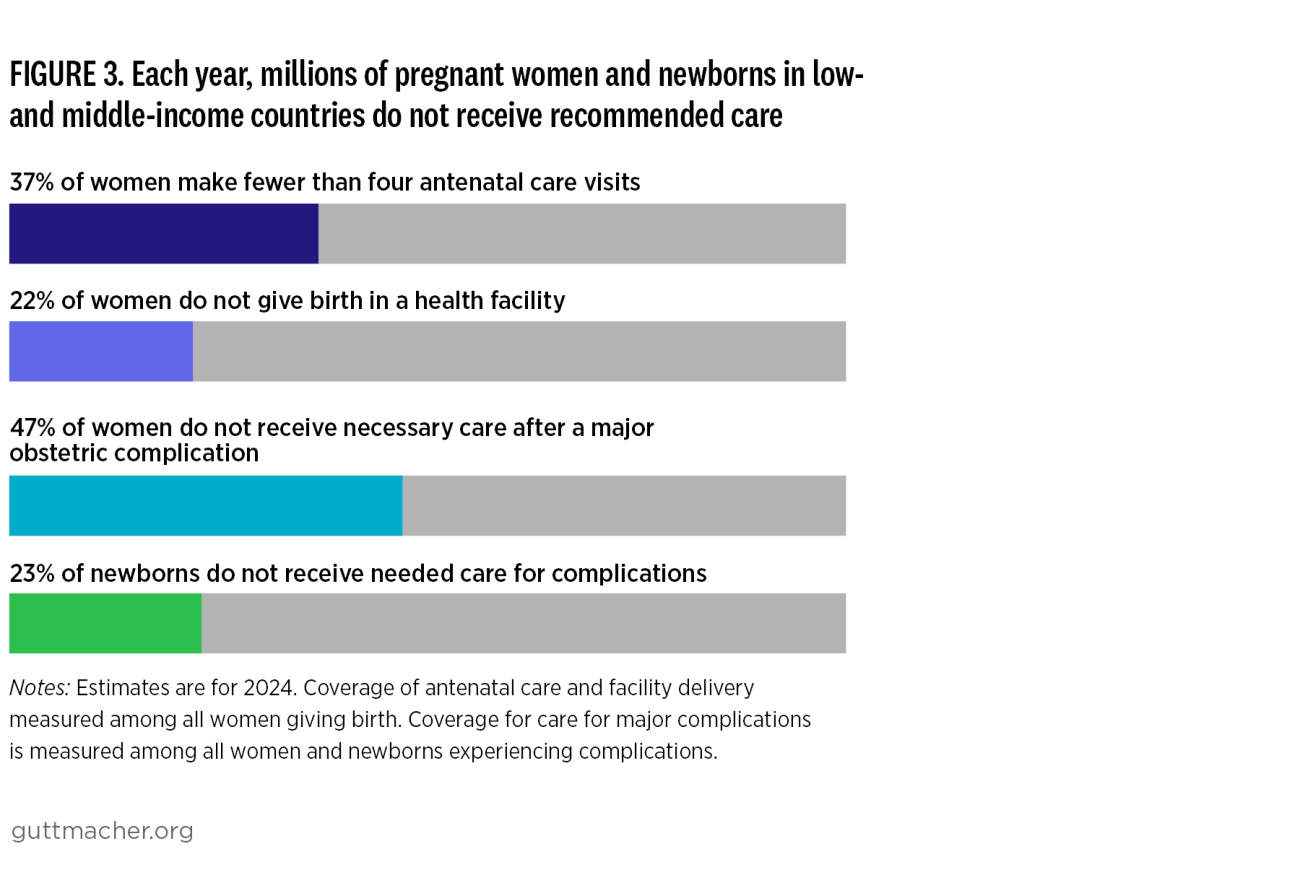
The estimates pertain to women of reproductive age (15–49) in 128 LMICs in 2024, and cover the following services: contraception, maternal and newborn care, abortion care and treatment for the major curable STIs. All cost estimates and savings are calculated in 2024 US dollars.
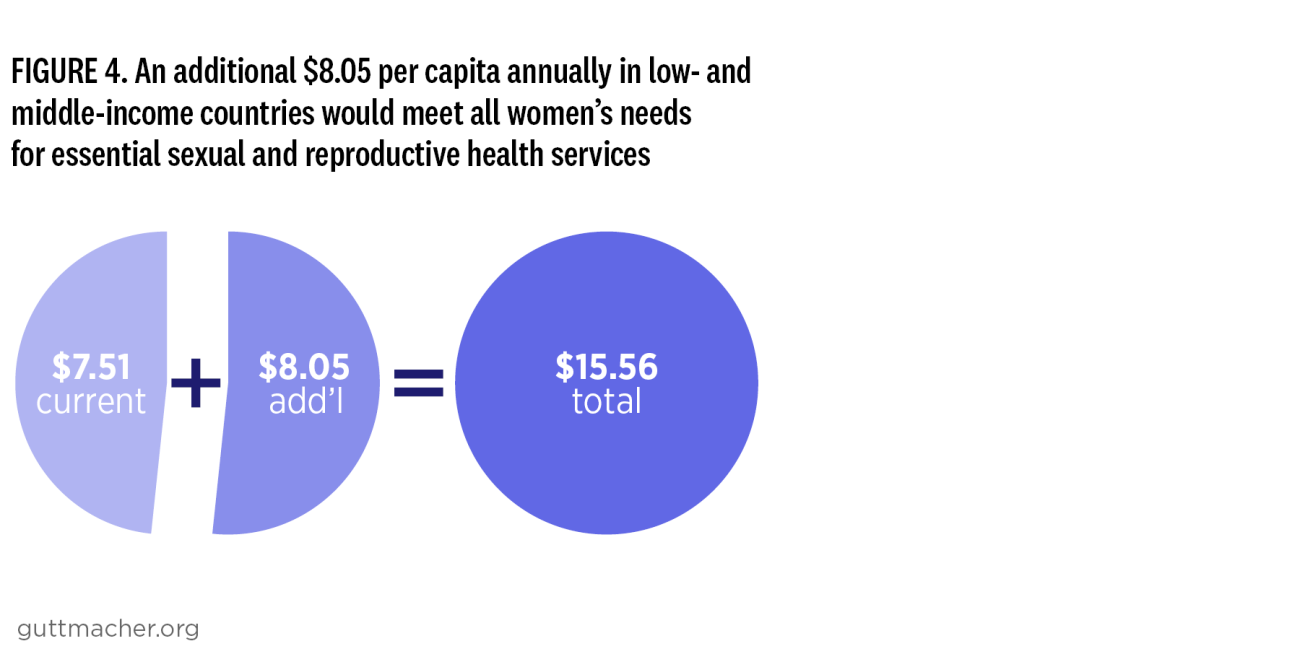
The need for robust estimates on sexual and reproductive health financing has never been more urgent. Funding is shrinking, and yet unmet need for care persists across LMICs, creating a widening gap between available resources and the investment required to meet women’s needs. In this increasingly constrained funding environment, evidence that accurately reflects women’s contraceptive needs and quantifies the true scale of financing gaps is critical in making the case for sustained and increased investment in contraceptive and broader sexual and reproductive health care.
New Estimates in Adding It Up 2024
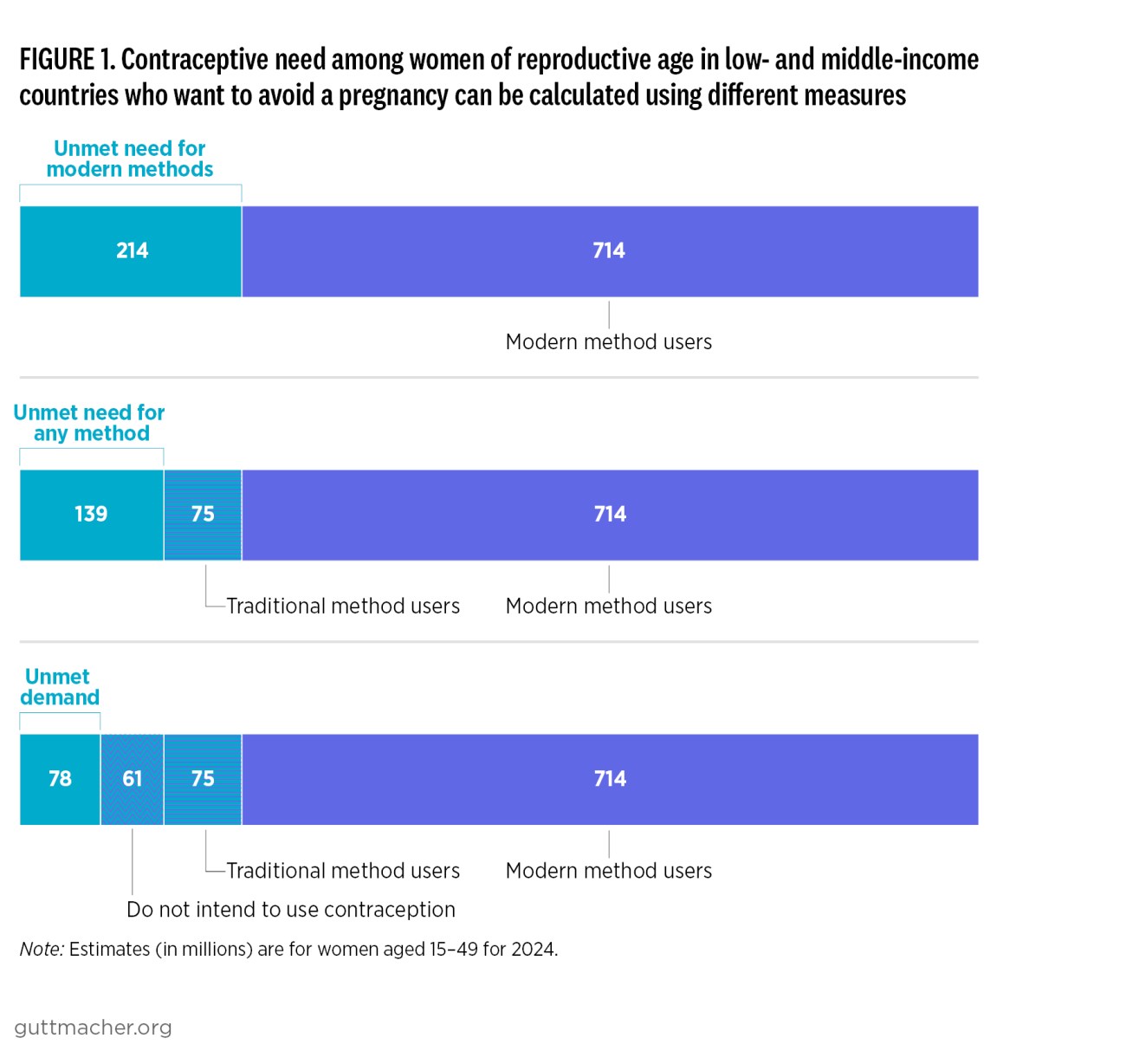
A major update in the 2024 Adding It Up study is how “unmet need” for contraception is defined. This new approach considers not only whether a woman is currently using modern contraception, but also whether she expresses interest in using it in the future. This shift creates a more person-centered way of measuring contraceptive need.
Why it matters: The calculation of unmet need helps determine how much additional funding is required for contraceptive services and, in turn, how many unintended pregnancies could be prevented with greater investment.
Previous approach: Earlier Adding it Up studies defined unmet need to include women who wanted to avoid pregnancy but were not using a modern contraceptive method. That measure assumed that all women in this situation wanted to adopt modern contraception, and it did not recognize that some women may already feel their needs are met by using traditional methods, such as withdrawal, abstinence or breastfeeding.*
New approach: The 2024 study provides three different ways to measure unmet need, from narrowest to broadest. The narrowest definition is called “unmet demand”1 and focuses specifically on women who want to avoid pregnancy and say they are interested in or open to using contraception in the future. This makes the estimates more grounded in women’s own preferences.