Published in 2019, this report provides the most current information on the incidence of unintended pregnancy and abortion in Kinshasa, Democratic Republic of Congo (DRC). Publication of the Maputo Protocol in the country’s legal gazette in 2018 formalized the government’s obligation to expand access to safe abortion within the terms outlined in the Protocol. Nevertheless, barriers to implementation continue to make safe abortion services largely inaccessible. As a result, the majority of women in Kinshasa who choose to end their pregnancies do so in secrecy—and often under unsafe conditions that endanger their health. This report summarizes the results of the 2016 Kinshasa Abortion Study, the first study to estimate the incidence of abortion in the DRC’s capital city. The report provides an estimate of the incidence of unintended pregnancy, documents the magnitude and severity of abortion-related morbidity, and elucidates the factors contributing to the risk of having an unsafe abortion.
Unintended Pregnancy and Abortion in Kinshasa, Democratic Republic of Congo: Challenges and Progress
Author(s)
Naomi Lince-Deroche, Patrick Kayembe, Nakeisha Blades, Crispin Mabika, Patrice Williams, Susan London, Jesse Philbin and Akinrinola BankoleReproductive rights are under attack. Will you help us fight back with facts?
Executive Summary
The penal code of the Democratic Republic of Congo (DRC) prohibits abortion, and although an article in the code of medical ethics permits it under very strict circumstances, safe services are largely inaccessible. Recent publication of the Maputo Protocol in the national gazette indicates that the legal status of abortion may shift toward liberalization, but implementation of this protocol will take time. As a result, the vast majority of women in Kinshasa who choose to terminate an unintended pregnancy will continue do so in secrecy—and often under unsafe conditions that may endanger their health and sometimes their lives.
Abortion is common in the DRC capital
- The 2016 Kinshasa Abortion Study, conducted by the Guttmacher Institute and the University of Kinshasa’s Department of Population and Development Studies and School of Public Health, is the first study to estimate the incidence of abortion in Kinshasa.
- An estimated 146,700 abortions took place in Kinshasa in 2016. The corresponding abortion rate—56 terminations per 1,000 women aged 15–49—is lower than rates among same- or similar-aged women in other major Sub-Saharan cities including Addis Ababa, Ethiopia (92 per 1,000 women); Kampala, Uganda (77); and Kigali, Rwanda (87); but it is higher than the rates for Nairobi, Kenya (32) and Dakar, Senegal (21).
- Among postabortion care patients who reported that they attempted to end their pregnancy, the most commonly used abortion method was misoprostol. More than half of women (56%) said they used misoprostol, and nearly half of this group used the medication in combination with another method.
Abortion in Kinshasa often has serious health consequences
- In 2016, an estimated 37,870 women in Kinshasa received care for complications resulting from abortion.
- According to the opinions of key informants knowledgeable about abortion in Kinshasa, 34% of women terminating a pregnancy likely have complications serious enough to warrant treatment in a health facility. Key informants thought that among this group of women, 77% receive the care they need, and 23% receive care somewhere other than a health facility or not at all.
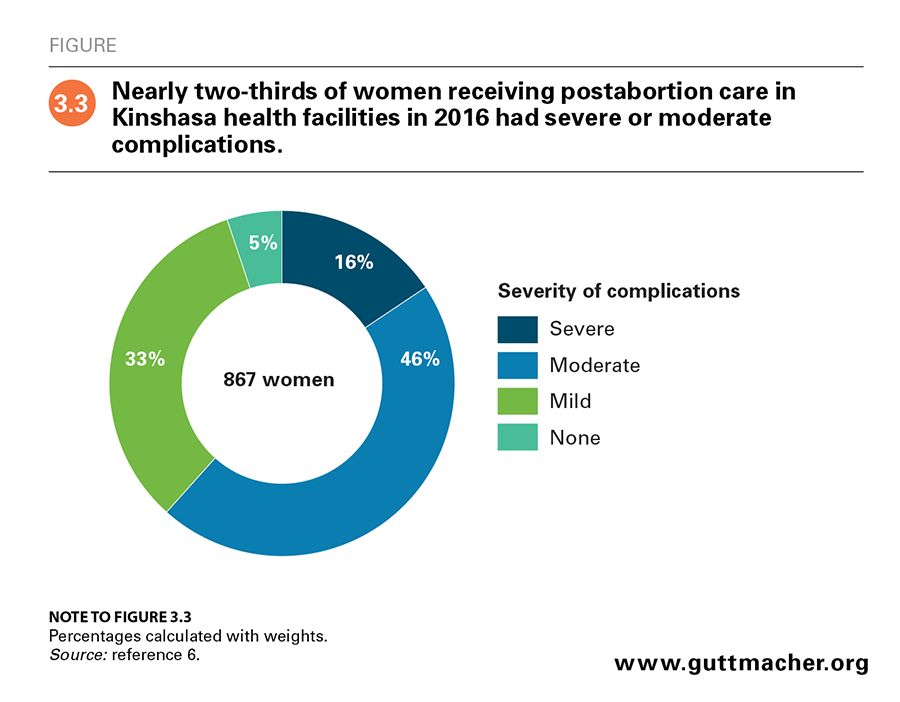
- Among all postabortion care patients, 5% had no evidence of complications, 33% had mild complications, 46% had moderate complications and 16% had severe complications, including shock, organ failure, generalized peritonitis and death. The postabortion care treatment rate for abortions was estimated to be 14 per 1,000 women aged 15–49.
- Nearly all postabortion care services in Kinshasa (93%) were provided in the private sector, where services are likely more expensive than at public facilities. This may be a barrier to care for women who need these services, especially for those who are socioeconomically disadvantaged.
- Among all women having an abortion, poor women were twice as likely as better-off women to have moderate or severe complications. Poor women were also thought to be less likely to receive postabortion care.
Unintended pregnancy is common in Kinshasa
- Of the estimated 563,100 total pregnancies in Kinshasa in 2016, 61% were unintended, corresponding to a rate of 147 unintended pregnancies per 1,000 women aged 15–49.
- Demographic and Health Survey (DHS) data indicate that women in Kinshasa have trouble meeting their fertility goals: In 2013–2014, women wanted an average of 3.6 children but had 4.2. In 2017, according to Performance Monitoring and Accountability 2020, unmet need for contraception was fairly high: One-quarter of married women had an unmet need for family planning.
- Barriers to contraceptive use in Kinshasa include individual-level characteristics—including young age and low socioeconomic status—as well as systemic challenges, such as lack of public education about contraception and limited method options at health facilities.
- Some 25% of women who reported experiencing violence during the pregnancy for which they required postabortion care indicated that the violence led to abortion. And among women who reported ever having experienced forced sex, 30% reported that the pregnancy for which they were seeking care was the result of this violence.
Action is needed to reduce levels of unintended pregnancy and unsafe abortion in the DRC
- Continuing recent efforts to improve access to and uptake of contraception will help women avoid unintended pregnancy and unsafe abortion. These efforts should include striving for improved quality and consistent availability of a broad range of methods in public facilities and ensuring that options are affordable and of acceptable quality. Services should be tailored to meet the particular needs of young women, and communities should be educated on method availability.
- Other root causes of unintended pregnancy and abortion, including gender inequality and violence against women, should also be addressed.
- The recent adoption of the Maputo Protocol holds promise for reducing unintended pregnancies and unsafe abortions in the DRC. Implementing the protocol, which requires signatory countries to allow abortion on broad grounds, will require considerable effort, including updating the penal code; training and equipping health professionals, including nurses and midwives, to provide safe abortions; and educating the population regarding access to services. Transitioning to legal services will also require reducing stigma, including by sensitizing health care providers and other stakeholders to women’s need for safe, nonjudgmental care.
- Given expectations for a long transition to full provision of safe abortion services, the capacity of Kinshasa’s health system, at both the primary and referral levels, should be strengthened to provide postabortion care services that meet international standards. Nurses and midwives should be trained to practice guideline-recommended manual vacuum aspiration and to use misoprostol for uncomplicated incomplete abortion.
- Improving the affordability of postabortion care services would also help to ensure that women who need those services receive them.
Context of Women’s Sexual and Reproductive Lives
The penal code of the Democratic Republic of Congo (DRC) prohibits abortion under all circumstances,1 and although abortion has long been tolerated informally, access to safe services is highly limited. An article in the code of medical ethics allows abortion to save a pregnant woman’s life (provided the termination is performed by a medical doctor and is approved by two other doctors),2 but it is likely that relatively few women are able to obtain a safe abortion via this avenue. As a result, the majority of terminations have been clandestine and therefore potentially unsafe. Also, because of its illegal status, abortion has been extremely hard to track or measure within the country, and the rate of unsafe abortion in the DRC and its capital has been a matter of speculation for many years.
However, the historic publication of the 2003 Protocol to the African Charter on Human and People’s Rights on the Rights of Women in Africa, also known as the Maputo Protocol, in the DRC’s national gazette in 2018 may mark a new openness on the part of the DRC government to liberalizing the abortion law.3 Described as "the continent’s foremost legal instrument on women’s rights,"4 the protocol stipulates that signatory states will protect women’s rights to abortion, to control their fertility and to choose any method of contraception, among other health-related rights. It further directs states to authorize abortion in cases of sexual assault, rape, incest or severe fetal anomaly, or if the woman’s life or physical and mental health are in jeopardy. It also obligates signatory states to protect other sexual and reproductive health rights.
By publishing the Maputo Protocol, the DRC government officially entered the treaty into legal force in the country, signaling a move away from the DRC’s total prohibition of abortion. Efforts will be needed to harmonize the country’s penal code with the Maputo Protocol to achieve a clear, consistent legal status for abortion and to establish mechanisms for ensuring that women who are legally allowed to have an abortion have access to the service. It will be some time before access to safe abortion services becomes a reality in the country. Until then, the vast majority of women ending unintended pregnancies will continue do so in secrecy—and some will use unsafe methods, untrained providers or both.
In the meantime, it is important to understand the extent to which abortion occurs in the DRC. To date, relatively little research has addressed the circumstances and consequences of unsafe abortion for those women who are unable to terminate their pregnancy safely. Also, the DRC is a large country, and national-level research is extremely hard to conduct. This report takes steps toward filling this information gap. The report summarizes the results of the 2016 Kinshasa Abortion Study (see box), the first study to estimate the incidence of abortion in the DRC’s capital city. In addition to covering abortion incidence in Kinshasa, the report:
- provides an estimate of the incidence of unintended pregnancy;
- documents the magnitude and severity of abortion-related morbidity; and
- elucidates the factors contributing to the risk of having an unsafe abortion by describing the characteristics of patients treated in health facilities for abortion-related complications.
The focus on Kinshasa should not be seen to imply that unsafe abortion is a problem needing attention only in this city. Where possible, the results of the research and the implications for policymaking and program planning are considered not only for Kinshasa, but for the DRC as a whole.
Data sources
The 2016 Kinshasa Abortion Study was undertaken jointly by the Guttmacher Institute and the University of Kinshasa’s Department of Population and Development Science and School of Public Health. The research team conducted surveys on abortion practices and postabortion care services with three groups: health facility representatives, knowledgeable key informants and postabortion care patients. The methodology for each survey is summarized below. Detailed methodologies and results from this work have also been published in two journal articles cited throughout this report.5,6
- Health Facilities Survey. This survey was conducted in Kinshasa in a representative sample of 361 public and private hospitals and health centers that treat women with abortion-related complications. At each facility, a senior staff member or administrator knowledgeable about the facility’s postabortion care services was asked to participate. At hospitals, respondents were usually obstetrician-gynecologists or the head of the obstetrics and gynecology department, and health center respondents were typically the director or a health care provider, such as a midwife or nurse. Data on the number of women who received postabortion care at each facility in 2016 were weighted to obtain a city-level estimate.
- Health Professionals Survey. This survey entailed interviews with 115 medical professionals, researchers, policymakers, advocates, social workers, NGO staff and other informed individuals, who were purposively selected for their knowledge of abortion provision and postabortion care in Kinshasa. Participants were asked for their opinions on the types of providers women in Kinshasa visit to obtain an abortion, the abortion methods used, the likelihood of complications, the proportion of women obtaining abortion who experience complications, and the proportion of women having complications who obtain treatment in a health facility. Participants were asked to provide responses separately for poor women and nonpoor women; however, they were not given an explicit definition of "poor."
- Prospective Morbidity Survey. This survey was based on interviews with a probabilistic sample of 867 women who received inpatient or outpatient postabortion care services following an unsafe abortion or a miscarriage in a representative sample of health facilities included in the Health Facilities Survey. Participants were asked about their reproductive history, socioeconomic and demographic characteristics, and experience with abortion or miscarriage. For women who consented, additional information on clinical diagnosis and treatment was obtained from the patient’s records and health care provider. Poverty status was indexed using questions on household possessions, following the approach routinely used in the DHS.7,8 The index was then standardized to match the distribution for Kinshasa in the 2013–2014 DHS because women receiving treatment for abortion complications were considered to be nonrepresentative of all women of reproductive age.
Throughout the report, data from the Kinshasa Abortion Study are complemented by city- and country-level data from the 2017 Performance Monitoring and Accountability 2020 survey and the 2013–2014 DHS.9,10
City- and country-level context
Kinshasa is the second most populous city in Sub-Saharan Africa.11,12 As of 2014, it was home to roughly 11 million inhabitants, or 13% of the DRC’s total population. Kinshasa’s population has grown at a rapid rate in recent years—an average of 4.2% annually between 2010 and 2015, outpacing the DRC’s growth rate of 3.3% between 2009 and 2016.12,13 Kinshasa is socioeconomically better off than the rest of the country, though the overall level of poverty is high.14
Throughout this report, evidence from Kinshasa is set against country-level context. As the country works toward improving access to safe abortion services, it will encounter significant developmental challenges. About three-quarters (77%) of the population of the DRC lives below the international poverty line of US$1.90 per day.15 The Human Development Index, which measures "three basic dimensions of human development (a long and healthy life, access to education, and standard of living)," ranks the DRC 176 out of 189 nations, placing it in the "low human development" category.16 Women in the DRC feel these disadvantages disproportionately. They obtain fewer years of schooling and earn less income than their male counterparts, thus scoring lower than men on the latter two dimensions of human development.
In many African settings, health and development indicators—including reproductive health indicators—tend to be better in capital cities than in the country as whole. According to the most recent DRC Demographic and Health Survey (DHS), in 2013–2014, data from women aged 25–49 show that the median age at marriage was 23 in Kinshasa, compared with 19 nationally.9 The median age of sexual debut among women aged 20–49 was 18 in Kinshasa, slightly more than a year older than the national median of 16.8. Among women aged 25–49, the median age at first birth was 22 in the capital city, compared with 20 for the country as a whole. Perhaps most strikingly, the proportion of 15–19-year-olds who had had a birth or were currently pregnant was 13% in Kinshasa, versus 27% for the nation overall.
Nearly nine in 10 women in the DRC aged 15–49 reported in 2013–2014 that they had heard of modern contraceptive methods (see box).9 However, only 8% of women nationally were using such methods. The proportion was higher among married women in Kinshasa (19%). Women in the DRC overall reported wanting an average total of 5.7 births, whereas women in Kinshasa wanted only 3.6. Still, given a national total fertility rate of 4.2, women in the capital had more children than they wanted in 2013–2014. Combined, these indicators point to the existence of widespread unmet need for contraception in the capital city. In other words, large proportions of women in Kinshasa are able to become pregnant and want to prevent pregnancy for at least two years but are not using a contraceptive method. In Kinshasa in 2013–2014, 23% of women who were married or in a union, 31% of sexually active unmarried women and 16% of all women were defined as having an unmet need for contraception.
Women’s challenges with regard to controlling their fertility are compounded by the DRC’s extremely high levels of violence against women. Starting in the early 1990s, the country experienced two decades of political instability and armed conflict (mostly centered in the eastern regions).17,18 Sexual violence was commonly used as a war tactic during those years and has remained commonplace. In 2011, researchers used 2007 DHS data to estimate the number of women nationally who had experienced rape and sexual violence perpetrated by an intimate partner. They estimated that 1.7–1.8 million women in the DRC had experienced rape in their lifetime, and more than 400,000 had been raped in the past 12 months—a figure that translates to four women having been raped every five minutes.19 More than three million women, or 35% of all women in the DRC aged 15–49, reported having experienced intimate partner sexual violence. In contrast, the proportion of women aged 20–44 reporting intimate partner sexual violence was 12% in Rwanda in 2005, 12% in Zimbabwe in 2005–2006 and 13% in Malawi in 2004.20
The most recent DHS provides updated information on rates of physical and sexual violence against women. In Kinshasa in 2013–2014, 57% of women aged 15–49 reported that they had experienced physical violence at least once since age 15, and their current or prior partner was the perpetrator in the majority of cases. Moreover, 21% of those women reported having experienced the violence "sometimes or frequently" in the past 12 months. The proportion of women reporting ever having experienced sexual violence was 27% in the DRC overall and 16% in Kinshasa, and the proportion reporting having experienced it in the past year was 16% and 6%, respectively.9 Although these numbers indicate improvement compared with the 2007 findings, the level of sexual violence throughout the country remains high. Violence, and in particular sexual violence, can expose women to an array of health risks.
Early sexual debut, high levels of contraceptive nonuse and experience of violence are among the factors likely to contribute to risk for unintended pregnancy and unplanned childbearing among women in Kinshasa.9 The few research studies that have looked at abortion in the DRC in the past indicated that women have obtained abortion in order to meet their fertility goals.21–23 A household survey conducted in Kinshasa in 1990 showed that 15% of women who had ever been pregnant had had at least one abortion,21 and in another household survey in 2006, 16% of women who had ever been sexually active reported that they had had at least one abortion.24 The studies also indicated that abortion has been particularly prevalent among adolescents. Interviews conducted in 2009–2010 with adolescent women residing in three outlying areas of Kinshasa revealed that 60% of 14–20-year-olds had previously self-induced a clandestine abortion.22 Respondents indicated that they were motivated to seek abortion because of fear that bringing a nonmarital pregnancy to term would bring stigma and damage their prospects for marriage; they also cited not being economically able to care for a child as a reason for choosing to terminate.
Definitions
This report adopts definitions used by the Demographic and Health Survey.
- Modern methods of contraception are female and male sterilization, contraceptive pills, intrauterine contraceptive devices (IUDs), injectables, implants, female and male condoms, diaphragms, contraceptive foams and jellies, lactational amenorrhea method, standard days method, cervical caps and contraceptive sponges.
- Traditional methods of contraception are periodic abstinence (rhythm and calendar methods), withdrawal, and folk and spiritual methods.
- Women with an unmet need for contraception are those aged 15–49 who are able to become pregnant but want to avoid pregnancy and are not using a method of contraception.
- Unintended pregnancies are pregnancies that were unwanted or mistimed at the time of conception.
Prioritizing sexual and reproductive health despite health system constraints
Prolonged instability in the DRC affected the country’s macroeconomic indicators by increasing inequality, slowing economic growth and straining resources.16,25,26 The 2001 Abuja Declaration committed African nations to spend 15% of their national budgets on health by 2015; yet, in 2009, health-related spending as a share of the national budget in the DRC was found to be equivalent to spending in 2000.27 Although the country did not meet the Abuja targets, progress was made: Between 2011 and 2015, spending on health as a proportion of the national budget rose from 3.4% to 8.6%, and 2015 marked the first year that the government set aside funding for essential drugs and contraceptives.28
Underfunding of health systems generally results in limited access to health services and poor health outcomes. In the DRC, underfunding of the health system combined with political instability was particularly detrimental to sexual and reproductive health. Although the country had a promising donor-supported family planning program in the 1980s, donor support ended when conflict set in, and it did not resume until the mid-2000s.18 Today, the vast size of the country and inadequate infrastructure, including transportation infrastructure, further contribute to poor health outcomes. In 2015, the estimated maternal mortality ratio was 27% higher in the DRC than the average for Sub-Saharan Africa: 693 maternal deaths for every 100,000 live births, compared with 546.29
Fortunately, the DRC’s current government has made improving sexual and reproductive health indicators a priority. In 2014, the country enacted its Family Planning National Multisectoral Strategic Plan.30 The plan’s six objectives are to obtain effective engagement from the government in favor of family planning, increase men’s and women’s access to family planning services in both the public and private sectors, improve the quality of services, increase demand for family planning, develop and reinforce an effective logistics management system for contraceptives, and implement a reliable evaluation system. The DRC has also made related commitments under the Family Planning 2020 initiative: In 2013, the country committed to increasing contraceptive prevalence to 19% (from a starting point of 5.4%) by 2020.31 It also created a budget line item for contraceptives and allocated $1 million annually. In 2017, the annual allocation was increased to $2.5 million dollars.32 More broadly, the country has committed to secure voting on a new law for sexual and reproductive health nationally, and to amend existing laws to "protect adolescent girls from early marriage through education, awareness raising, social reintegration, and women’s empowerment."32(p.2)
Finally, the government of the DRC took a strong step toward improving access to sexual and reproductive health services—including safe abortion services—when it published the Maputo Protocol. As the country begins harmonizing its laws and taking steps toward establishing access to safe abortion services, taking stock of current abortion practices is important for understanding what must be prioritized.
Incidence and Practice of Abortion
Data from the 2016 Kinshasa Abortion Study’s Health Facilities Survey and Health Professionals Survey indicate that approximately 146,700 abortions took place in Kinshasa in 2016.5 This corresponds to a rate of 56 abortions per 1,000 women aged 15–49, and an abortion ratio of 44 abortions per 100 live births, or slightly more than two pregnancy terminations for every five births. A study published shortly after the 2016 Kinshasa Abortion Study supports these findings. The researchers used a different approach, the confidante method, where women are asked about abortions obtained by women who confide in them. The resulting abortion rate using this method was 55 abortions per 1,000 women aged 15–49.33
Kinshasa’s abortion rate is lower than rates found in other Sub-Saharan capital cities, such as Addis Ababa (92 per 1,000 women),34 Kampala (77)35 and Kigali (87),36 and it is higher than the combined rate for Nairobi and the Central Region in Kenya (32)37 and the rate for Dakar (21).38 The abortion rate for the DRC as a whole is unknown, but rates are often elevated in capital cities, compared with less populated areas. This is true for a few reasons: Urban areas typically offer greater access to health services generally, and individuals in rural areas travel to cities to obtain services.34 Also, people in urban areas also tend to have lower desired fertility than people in rural areas.5 Lastly, the relatively liberal social views typically found in urban areas may extend to social norms that are more accepting of abortion.
Abortion practice in Kinshasa
Previous research has shown that women in the DRC may attempt to induce abortion with traditional methods, for example, by using cimpokolo and other herbs, quinine, or other oral medicines obtained from friends, family and traditional practitioners.39,40 In addition, providers and pregnant women are known to terminate pregnancies clandestinely using misoprostol.41 Misoprostol, which is registered in the country as a treatment for gastric ulcers under the brand name Cytotec, is a safe and effective means of inducing abortion when administered with proper guidance, but access to the drug is not yet widespread.
In the 2016 Kinshasa Abortion Study’s Health Professionals Survey, key informants knowledgeable about sexual and reproductive health, including health care professionals, health facility administrators, educators and community outreach activists, reported their opinions on the methods used to terminate pregnancies.42 According to these interviews, a wide range of methods are used to induce abortion in Kinshasa. At least nine in 10 key informants agreed that dilation and curettage (D&C) and overdoses of pharmaceutical drugs such as quinine, antiparasitics and antibiotics are used. Oral and vaginal use of misoprostol were reported by about four-fifths of key informants. Sizeable majorities also reported that manual vacuum aspiration, electric vacuum aspiration and traditional methods (such as oral and vaginal use of herbal remedies) are used. About half mentioned that abortion is sometimes induced using sharp or pointed objects (such as broom handles or sticks), while two in five respondents mentioned oral intake of hormonal medications or injections of drugs (such as quinine and oxytocin).
According to the key informants’ opinions, the method used to induce an abortion varies by provider or source. Doctors, clinical officers and nurses most commonly perform D&C, while traditional practitioners most commonly administer oral herbs and decoctions, and pharmacists offer misoprostol. Pregnant women attempting to self-induce abortion were thought to rely mainly on misoprostol, and key informants noted that the majority of women using misoprostol obtain it from public or private health facilities, providers’ homes or pharmacies. Finally, other untrained providers were thought to most often use vaginal insertion of sharp or pointed objects to induce abortion.
The World Health Organization recommends medication abortion using a combination of mifepristone and misoprostol (or misoprostol alone where mifepristone is not available, as in the DRC) or surgical abortion using vacuum aspiration for first-trimester abortions (as well as for most later abortions).43 They no longer recommend D&C for use at any gestation, as it is slower, more painful and less safe than the alternatives. The apparent widespread use of D&C by health professionals in Kinshasa is contrary to best practices and may contribute to women’s experience of abortion complications.
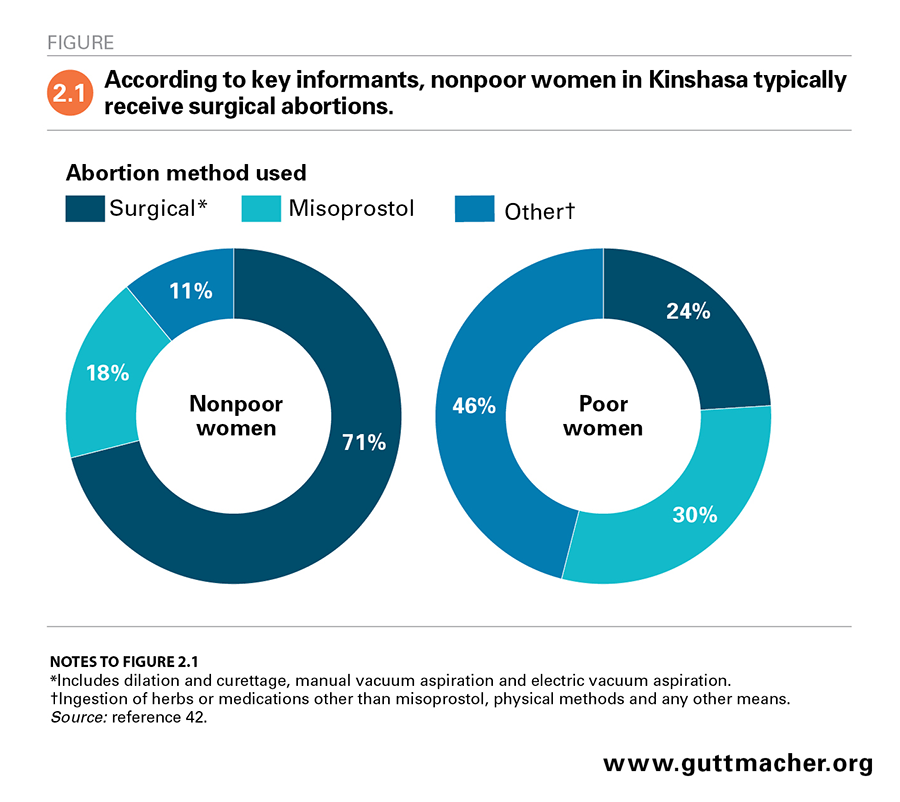
A woman’s socioeconomic status was thought to determine the type of abortion care she receives. Key informants were asked to estimate what proportions of poor and nonpoor women undergo each type of abortion and go to each type of provider; informants’ responses were then averaged to obtain an overall estimate. According to key informants, nearly three-quarters (71%) of nonpoor women who terminate a pregnancy obtain a surgical procedure (D&C or vacuum aspiration), 18% use misoprostol and 11% rely on other methods, including those offered by untrained providers (i.e., ingestion of herbs, use of medications other than misoprostol or vaginal insertion of objects; Figure 2.1).42 In contrast, 24% of poor women having an abortion were thought to obtain surgical procedures, 30% to use misoprostol and 46% to use other methods.
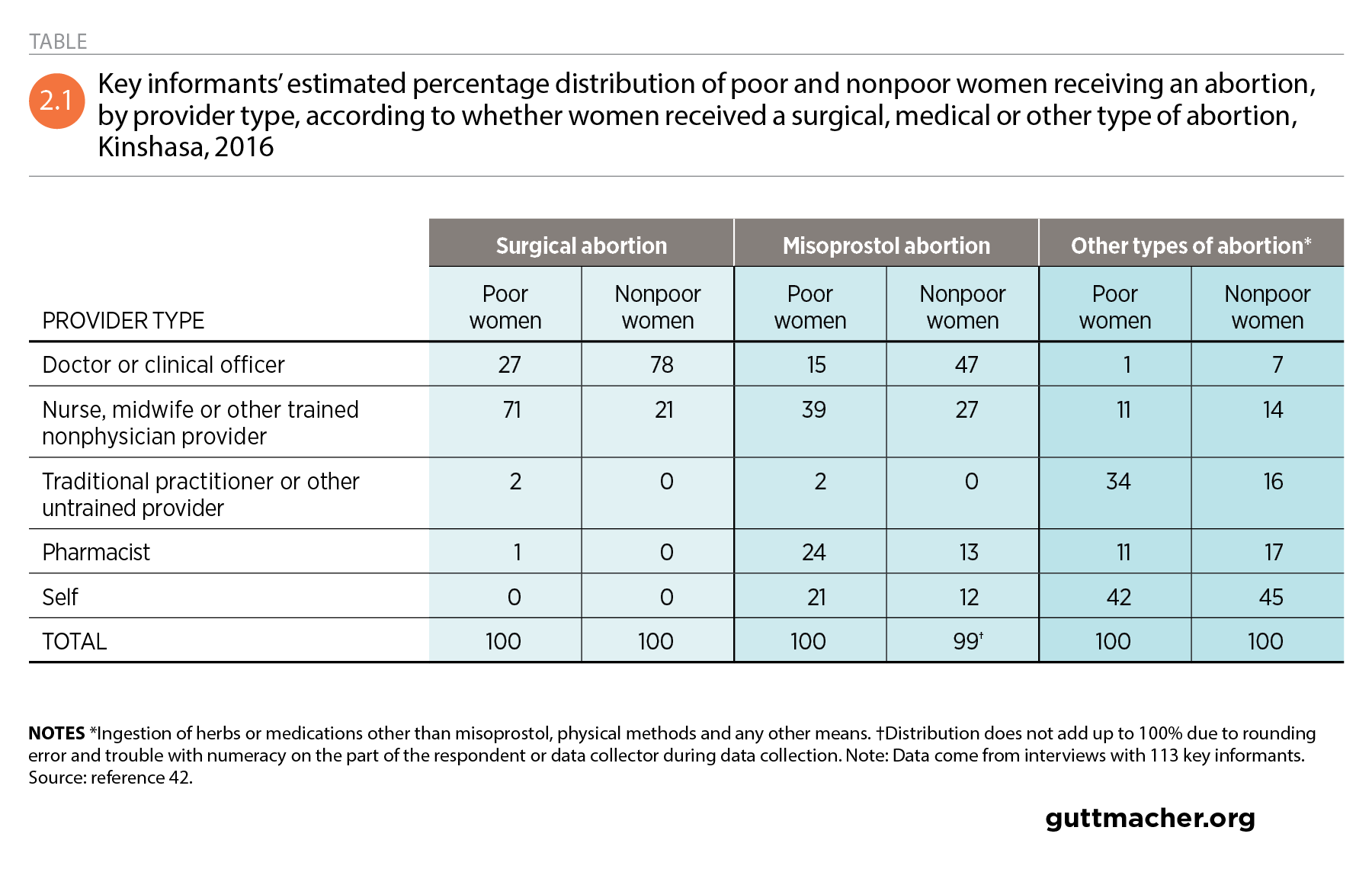
Key informants estimated that nearly three-quarters of poor women having a surgical procedure consult trained nonphysician health care providers, such as nurses or midwives, and 27% go to a doctor or clinical officer (Table 2.1).42 For nonpoor women, these proportions are nearly reversed: An estimated 78% obtain surgical abortions from a doctor, while the remainder use other trained providers. For misoprostol abortions, key informants estimated that two-thirds of poor women consult trained nonphysician medical providers or pharmacists, while about half of nonpoor women go to doctors or clinical officers. Some 21% of poor women and 12% of nonpoor women obtain and use misoprostol on their own.
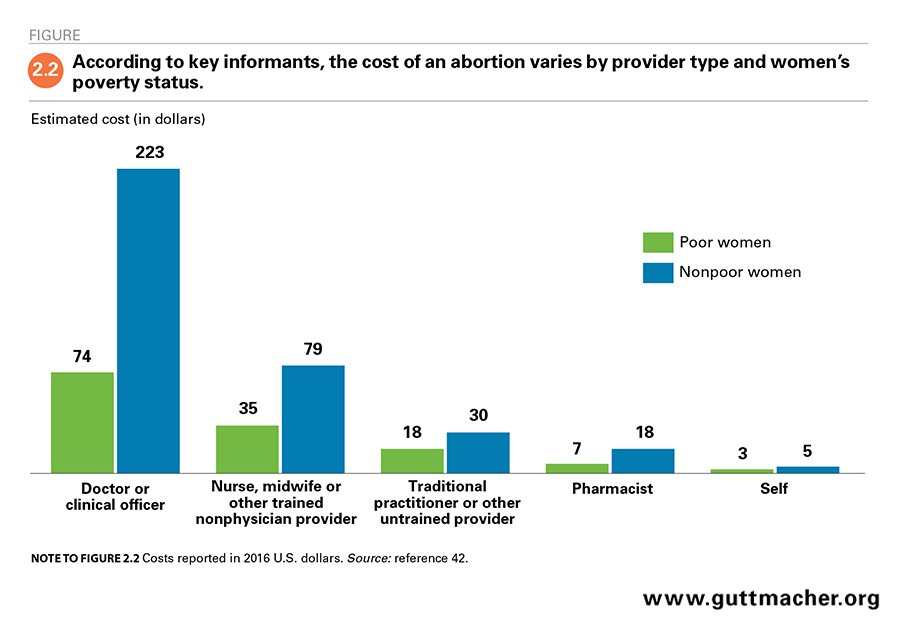
According to key informants, medical doctors and clinical officers are generally the most expensive abortion providers, and terminating a pregnancy on one’s own is the least costly option (Figure 2.2).42 However, the amount a woman pays for an abortion varies according to her poverty status. For an abortion obtained from a doctor or clinical officer, poor women were estimated to pay $74 (based on the average of key informants’ responses),* whereas nonpoor women were thought to pay roughly three times as much ($223). The difference in estimated cost across socioeconomic groups shrinks as the skill level of the provider decreases. Nonpoor women were thought to pay approximately twice as much as poor women do for an abortion from a nonphysician provider ($79 vs. $35) and a little less than twice as much as poor women do to obtain the procedure from a traditional practitioner or other untrained provider ($30 vs. $18). Terminating a pregnancy on one’s own was estimated to cost about $5 for nonpoor women and $3 for poor women.
Women’s reports of their abortion experiences
The 2016 Kinshasa Abortion Study’s Prospective Morbidity Survey asked women receiving facility-based postabortion care whether their pregnancy had ended as a result of something they or someone else had done. About two-fifths of interviewees responded affirmatively to this question.44 However, it is known that women commonly underreport abortion because of stigma.45–47 Thus, researchers in the 2016 Kinshasa Abortion Study applied a classification system, initially developed by the World Health Organization, that incorporates both self-reporting from the woman and observations by a health care worker (Appendix Table 1, download above).48 Based on that system, the researchers estimated that 72% of postabortion care patients interviewed in the 2016 Kinshasa Abortion Study had had an abortion.6
Among women classified as having had an abortion, 81% indicated that they did not intend to become pregnant at the time they conceived.44 These 452 women (who reported that they did not want, wanted later, or did not know if they wanted the pregnancy for which they were obtaining postabortion care) reported a number of reasons for wanting to avoid a pregnancy, including being unmarried (42%), wanting to maintain family honor (23%), financial considerations (22%), fearing being kicked out of the home (21%), health concerns (19%), wanting to space their births (19%), being too young to have child (15%), having enough children already (13%), opposition from family (11%) or opposition from their partner (11%; Figure 2.3). Most of these reasons were also cited by the small group of women who expressed that they initially wanted the pregnancy but later changed their mind.
Nearly half (44%) of women who were classified as having had an abortion reported that they discussed interrupting the pregnancy at some point prior to obtaining care in the facility (data not shown).44 Most commonly, women spoke about this with their partner (73%), a friend (33%) or a female relative (31%). The majority of these women (83%) reported that at least one person they consulted thought the woman should end her pregnancy.
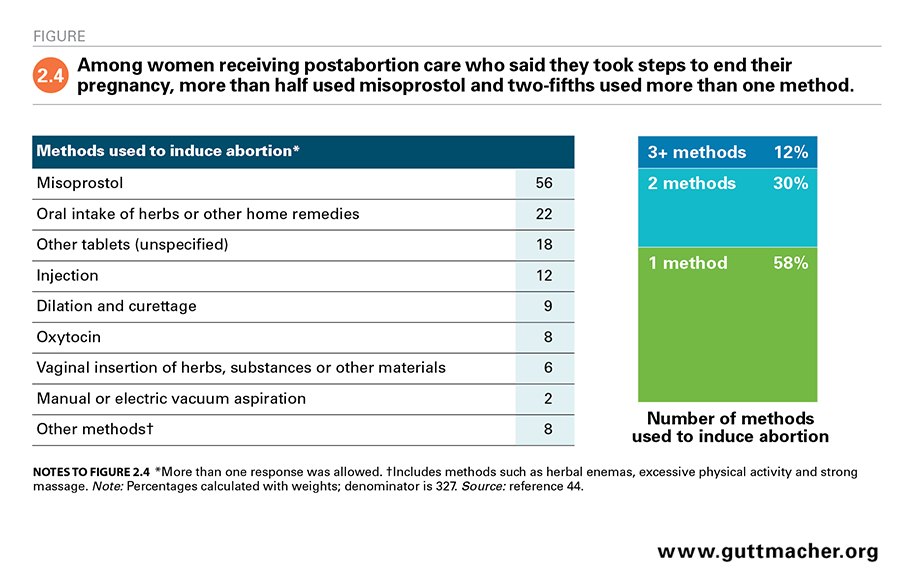
Three-fifths of the women classified as having had an abortion explicitly reported that they took some action to end their pregnancy. Two-fifths of these women indicated that they made the decision to do so alone, while the others most often consulted their partner.44 About two-fifths of the women who said they took action end to their pregnancy used more than one method to terminate their pregnancy, and some reported using as many as five methods (Figure 2.4). More than half (56%) reported using misoprostol, either as the only method they used to stop the pregnancy (31%; data not shown) or as one of several methods employed (25%).
It is important to note that Prospective Morbidity Survey data represent the subset of women with complications from unsafe abortion who managed to obtain care in a health facility. While we believe that the decision-making patterns and reasons for pregnancy termination among this group are unlikely to have differed from those of women with uncomplicated abortions or untreated complications, the abortion methods used by these groups of women are likely to have been different. For example, women with uncomplicated abortions may have used safer termination methods than the women captured in this survey.
Health Consequences of Unsafe Abortion and Postabortion Care
An estimated 6.2 million unsafe abortions occurred each year in Africa in 2010–2014,49 and 69% of all abortions in Middle Africa—the subregion that includes Kinshasa—are categorized as least safe (as opposed to safe or less safe†). That means the majority of abortions in Middle Africa are performed by untrained providers and are done using unsafe methods. Nineteen percent of abortions in Middle Africa are categorized as less safe—that is, they are performed by untrained providers or with unsafe methods. Only 12% of abortions in the region are considered safe.
Due to its high level of unsafe abortion, Africa is the continent with the highest abortion-related case-fatality rate, at 141 deaths per 100,000 abortions.50 Africa accounts for 29% of all unsafe abortions but 62% of all deaths from unsafe abortion worldwide.49 In 2017, an estimated 7% of maternal deaths in Sub-Saharan Africa were related to abortion.51 This translates to the largely preventable loss of about 14,600 lives; 3,000 of these deaths occurred in Middle Africa. Studies from African settings have shown that at the household level, maternal death—from unsafe abortion or other causes—may result in economic insecurity; poor infant and child health; and decreases in income, education and opportunity.52–56 These negative outcomes of unsafe abortion have ripple effects on the welfare of communities and countries.57,58
While death is its most serious consequence, unsafe abortion can lead to a range of complications, some of which require medical attention to prevent short- and long-term pain and disability, and reduced quality of life.59,60 Postabortion care encompasses a package of vital health care services targeting the particular needs of women experiencing complications from abortion and miscarriage. Estimates for 2014 show that fully meeting the need for postabortion care in developing regions would have dramatically reduced deaths related to unsafe abortion from 22,000 to 9,000 per year.61 In addition, full provision of postabortion care would have vastly improved women’s well-being by reducing the number of years of healthy life lost to abortion‡ from 1.5 million to 600,000 per year.
Postabortion care in Kinshasa
The 2016 Kinshasa Abortion Study sheds light on the city’s need for and access to postabortion care.5 After adjusting for patients who may have been double-counted as a result of having been referred from one health facility to another and women known to have come from outside the city, it was estimated that 49,090 Kinshasa-based women received postabortion care for abortion or miscarriage. Of those, 37,870 women were treated for complications resulting specifically from abortion, meaning that 77% of all women who received postabortion care in Kinshasa in 2016 required care for complications from unsafe abortion. The postabortion care treatment rate was 14 women treated per 1,000 women aged 15–49.
Key informants in the Health Professionals Survey provided estimates of the proportion of women who needed postabortion care but did not receive it. Based on key informants’ knowledge of methods used to induce abortion, method safety and the likelihood that women who have abortion complications obtain postabortion care, they estimated that 34% of women terminating a pregnancy likely have complications serious enough to warrant treatment in a health facility.42,62 The key informants thought that among this group of women, 77% receive the facility-based care they need. The other 23% (about 11,500 women) either obtain care outside the formal health care system (from medical professionals or from traditional practitioners) or they go without care altogether.
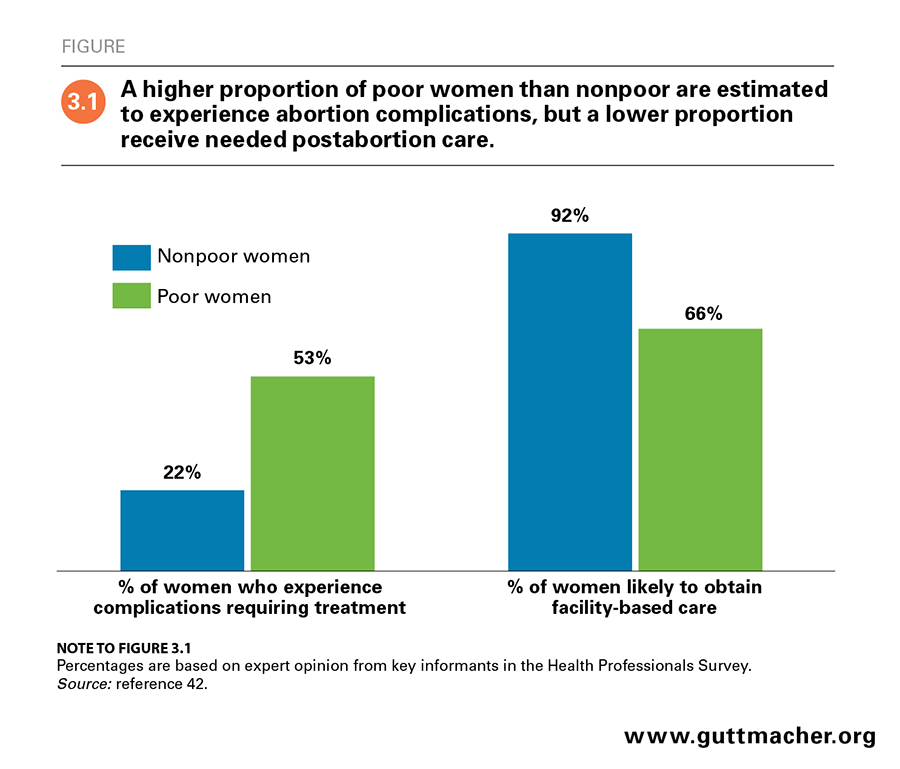
Key informants in the Health Professionals Survey also suggested that the need for and use of postabortion care varies by socioeconomic characteristics, reflecting significant inequities in access to health care and outcomes. They estimated that about half of poor women having an abortion experience complications requiring treatment, compared with 22% of nonpoor women (Figure 3.1).42 Among those who experience complications, key informants suggested that nearly 66% of poor women obtain facility-based care, compared with 92% of nonpoor women. Therefore, an estimated 18% of those who are poor experience complications that are not treated in a health care setting, compared with just 2% of nonpoor women.
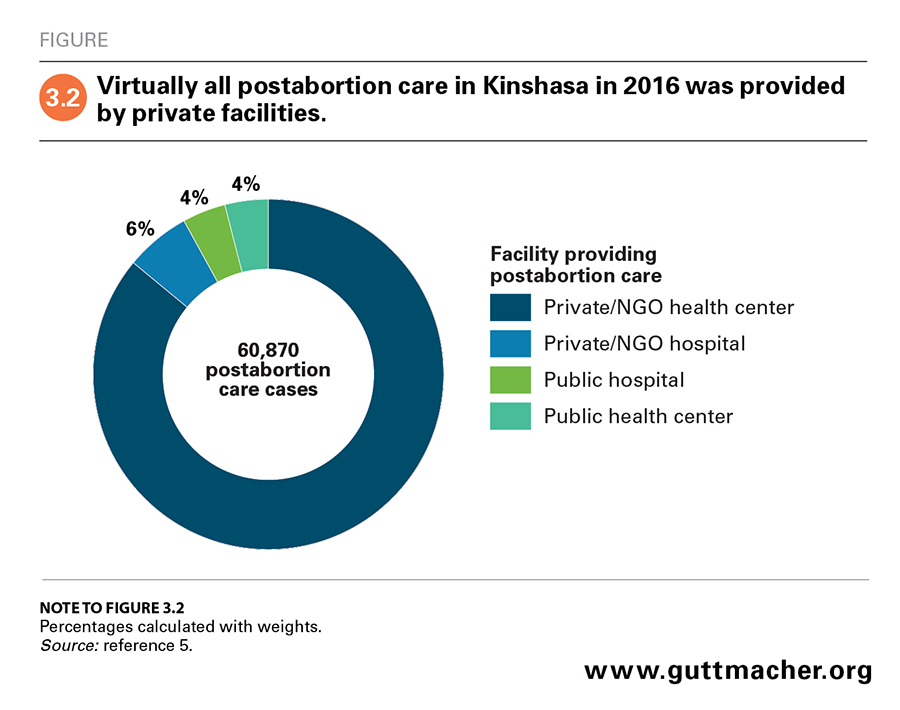
Health Facilities Survey data show that nearly all postabortion care in Kinshasa (92%) is provided in private-sector facilities (including in NGO facilities; Figure 3.2), and the out-of-pocket costs for care in these facilities are likely higher than at public facilities.5 Though the facility with the highest annual postabortion care caseload (252 women) was a public hospital, slightly fewer than 8% of cases overall were treated in public hospitals and health centers.
Characteristics of patients receiving postabortion care
Very little past research has described the characteristics of women obtaining postabortion care in the DRC generally or in Kinshasa specifically. One such study reported on a cohort of women treated for complications of illegal abortions in university clinics in Kinshasa in 1978–1979.63 Among women who illegally ended their pregnancy, two groups were disproportionately represented: women younger than 20 experiencing a first or second pregnancy who were unmarried, currently in school or poor; and women aged 20 or older who were married, educated and economically active. All of the patients were deemed to have had the procedure before 12 weeks’ gestation, usually with unqualified providers. A second study, conducted in Kinshasa in 2014, captured information on women admitted to the emergency obstetrics wards of five large referral hospitals.64 Among the women admitted, nearly 15% had abortion complications. The majority of the patients were married or cohabiting, had had more than one birth and reported no prior abortions. Also, adolescents and nonmarried women were more likely to have been admitted for complications from abortion than older patients or married women, respectively.
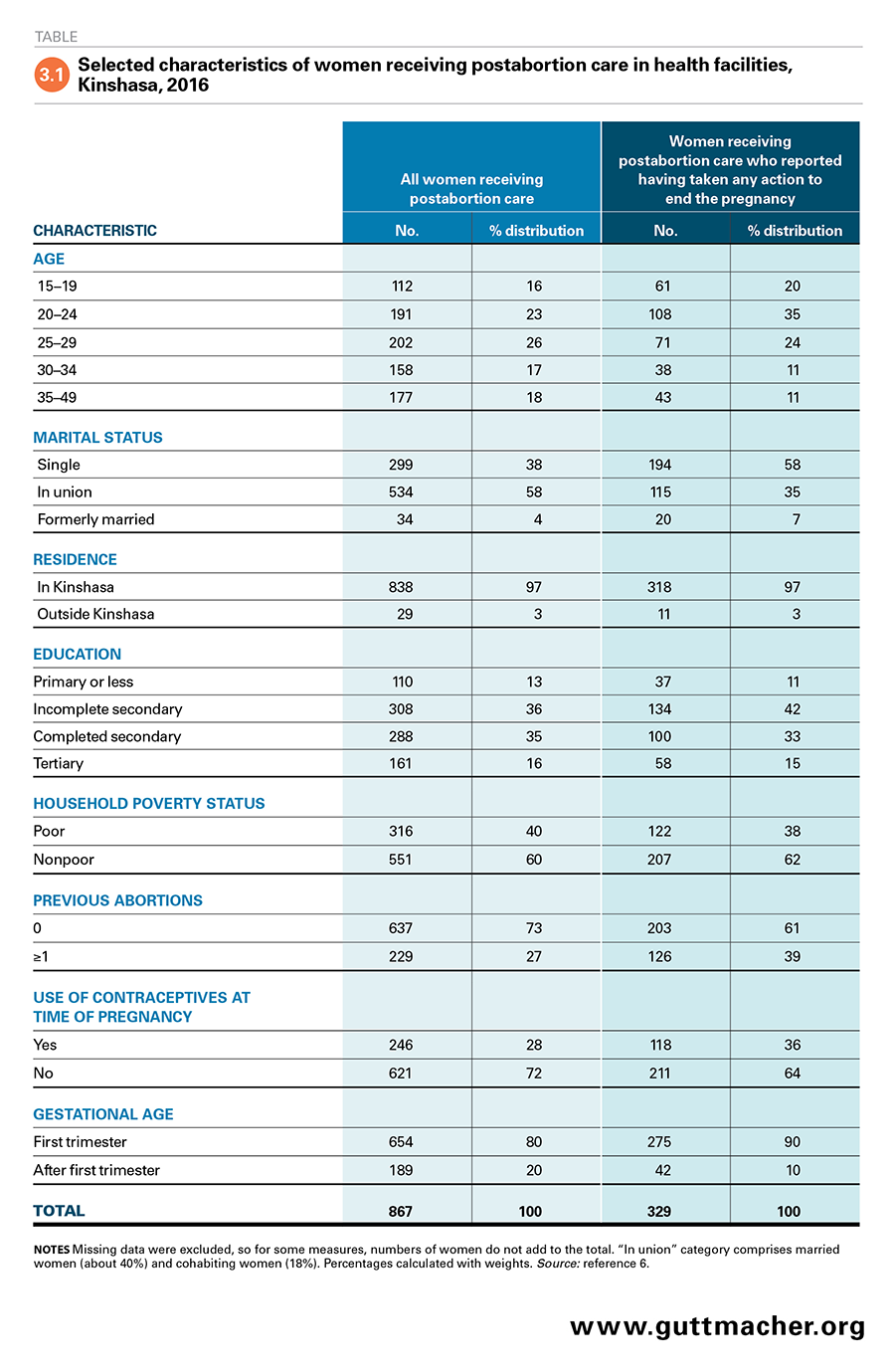
The 2016 Kinshasa Abortion Study’s Prospective Morbidity Survey sheds additional light on the characteristics of women receiving postabortion services, drawing data from interviews with women who obtained care after an abortion or miscarriage. At the time they were interviewed, half of the surveyed women were in their 20s, 35% were aged 30 or older and 16% were adolescents aged 15–19 (Table 3.1).6 More than half were in union (58%), and a sizable majority (87%) had at least some secondary education. Four in 10 were poor. More than a quarter (28%) of women obtaining postabortion care reported they were practicing contraception when they became pregnant, and the large majority reported having been in their first trimester of pregnancy (81%) at the time of the abortion or miscarriage. The majority of women receiving postabortion care also reported having had at least one previous pregnancy (81%) and indicated that they had at least one child (69%; data not shown).6,44 About one-quarter (27%) reported at least one previous abortion.6
The subset of patients who explicitly reported having had an abortion tended to be younger than postabortion care patients overall.44 Nearly three-fifths (59%) of women who reported having ended their pregnancy were in their 20s, while adolescents and women aged 30 and older each accounted for a fifth. Considerable proportions were single (58%), were using contraceptives when they conceived (36%), were in their first trimester (90%) and had had at least one prior abortion (39%).
Severity of complications treated
The Prospective Morbidity Survey classified postabortion care patients by the severity of their abortion complications (see Appendix Table 2 for classification criteria, download above).6 Five percent had no evidence of complications and most likely sought medical intervention unnecessarily, 33% had mild complications, 46% had moderate complications, and the remaining 16% had severe complications such as shock, organ failure, generalized peritonitis and death (Figure 3.3).
The severity of complications varied by women’s socioeconomic, demographic and clinical characteristics.6 The odds of having had moderate or severe complications were 49% lower among women aged 20–24 than among those aged 35 and older. Furthermore, the odds of having severe complications were 71% lower among women aged 25–29 than among those aged 35 and older. Poor women and those who had had an abortion had approximately double the odds of having experienced moderate or severe complications, compared with better-off women and those who had a miscarriage, respectively. Single women and cohabiting women had twice the odds of having had moderate or severe complications, compared with their married or previously married peers. Those who reported being past their first trimester of pregnancy when the pregnancy ended had odds of having a severe complication that were 3.7 times those of women having a first-trimester procedure. Finally, the odds of having had severe complications were half as high among women who had a previous abortion than among those who had no previous abortion experience.
New insight into postabortion care services
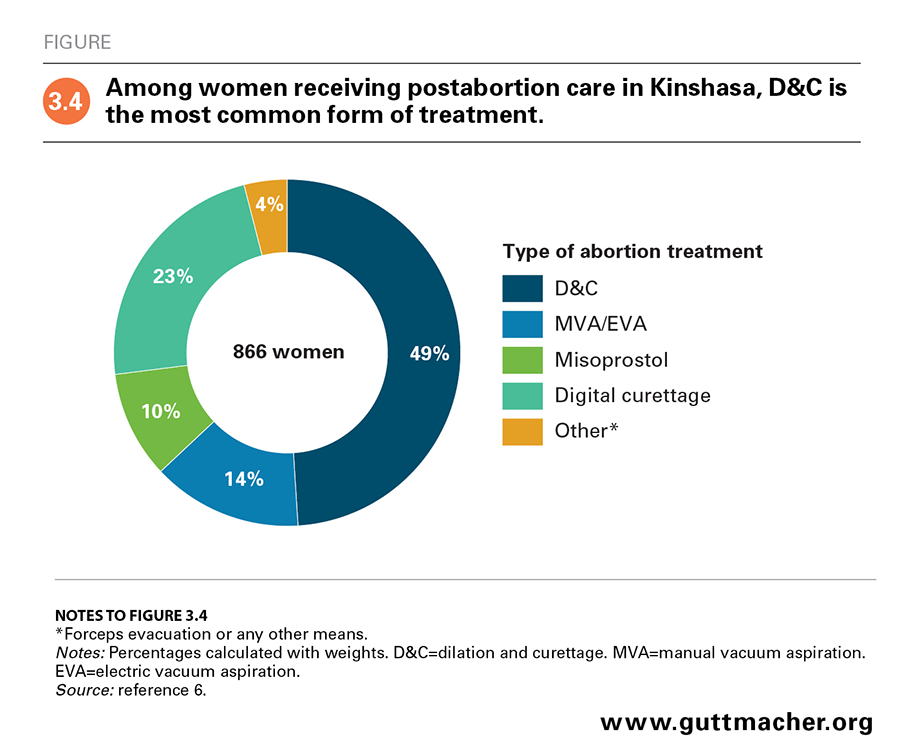
The Prospective Morbidity Survey also collected 2016 data on the type of services received by women undergoing postabortion care. About half (54%) of women presenting for postabortion care were treated by doctors, who are the providers most likely to treat women with severe complications.6 Despite the fact that dilation and curettage (D&C) is not recommended by the World Health Organization, it was the most commonly performed technique for women receiving postabortion care (used in 49% of cases; Figure 3.4). Digital curettage was used for 23% of postabortion care patients, manual and electric vacuum aspiration for 14%, and misoprostol and other methods for the remaining 14% of cases. D&C was more commonly used for women in their first trimester (51%) than for those in their second and third trimesters (43%; data not shown).44
Just 11% of women receiving postabortion care were given pain medication. Receipt of pain medication was slightly more common among women with severe complications (15%) than among those with no complications (9%) or mild complications (11%).6 The practice of not offering pain medication has also been documented in settings where safe abortion services are provided, and data suggest it could be due to bias against women who have terminated a pregnancy.65
Finally, just 15% of patients in the 2016 Kinshasa Abortion Study’s Prospective Morbidity Study received contraceptive methods at the time of discharge; 16% were referred elsewhere for contraceptive services. Provision of contraceptives was more common among women with severe complications (20%) than among those with no or mild complications (13%).6
Factors Contributing to Unsafe Abortion
Understanding how to curb morbidity and mortality resulting from unsafe abortions requires understanding its causes. Globally, the rate at which safe or unsafe abortions occur in a given setting is influenced by a range of factors. These include women’s fertility preferences, patterns of contraceptive use and nonuse, women’s motivation to avoid carrying an unintended pregnancy to term, and their ability to act on their preferences given the legal, structural and social context.66
Contraceptive use and barriers to use
Demographic and Health Survey (DHS) data for 2013–2014 show that use of modern contraception among women in the DRC was low and unmet need for contraception was high.9 Just 8% of married women and 21% of sexually active unmarried women in the country were currently using a modern contraceptive method, and modern methods were used by 19% of married women in Kinshasa. Twenty-three percent of married women in the city had an unmet need for contraception; most of these women had a need to space their births, rather than to prevent or cease childbearing. In addition, a sizable share of married women in Kinshasa (26%) were relying on traditional methods of family planning. Just 28% of the contraceptive need among married women was satisfied using modern methods. Unmet need among sexually active unmarried women in Kinshasa was 31%, and 30% of contraceptive need in this group was satisfied using modern methods.
Individual- and household-level characteristics are important contributors to contraceptive uptake. According to national data from the 2013–2014 DHS, contraceptive prevalence (i.e., use of modern or traditional methods) was higher among women with more education and those in wealthier households than among women who were less educated and poorer.9 In a 2006 study conducted in Kinshasa, having ever used a modern method and having discussed contraception with anyone in the previous 12 months were associated with greater uptake.24 Use also varied with age: Adolescents aged 15–19 knew less about modern methods and were consequently less likely to use them than older age-groups. Interestingly, data from a nationally representative study in the DRC in 2015 indicated that individuals’ exposure to sexual violence from an intimate partner was positively associated with current modern method use, whereas exposure to other conflict was not (possibly because of poor access in conflict-ridden areas).67
Structural and environmental factors also play a role in women’s and couple’s use or nonuse of contraceptives. In qualitative interviews conducted in six provinces in the DRC, men and women reported that lack of access to information is a barrier to contraceptive use.68 Respondents specifically mentioned fear of side effects, lack of knowledge about the types and sources of contraceptive methods, and misinformation—all of which reflect shortcomings in the provision of information in health facilities and elsewhere. The cost of a consultation or supplies associated with a contraceptive visit can also hinder access. In the 2013–2014 DHS, 57% of women using a modern method reported that they obtained their method in a private facility, usually a pharmacy, and this suggests that even though free or subsidized contraceptive services exist in the DRC, most women are not accessing this type of care.9
Also, many women may find that the methods or services they need are unavailable at public or private facilities. In the 2014, 2015 and 2016 Performance Monitoring and Accountability 2020 surveys, one-fifth of public and private health facilities and pharmacies in Kinshasa that reported offering family planning services did not actually offer services on the day of the survey.69 The 2016 survey showed that only half of facilities offering family planning had three or more methods available, and more than a quarter of those facilities reported having had a stock-out of all methods except condoms in the previous three months.
Despite challenges, there is evidence that the level of contraceptive use in Kinshasa may be on the rise. Although contraceptive uptake improved little between the 2007 DHS and the 2013–2014 DHS,9 the 2017 Performance Monitoring and Accountability 2020 survey estimated that 41% of all women in the city were practicing some form of contraception and 22% were using modern methods.10 Among married women, the proportions were 47% and 27%, respectively. Unmet need in that year stood at 16% among all women and 25% among married women.
Unintended pregnancy
Among women who do not wish to become pregnant, nonuse of contraceptives and contraceptive failure may result in mistimed or unwanted pregnancy. And faced with an unintended pregnancy, many women seek abortion or give birth to a child they had not planned for: Data from the DHS in 2013–2014 indicate that women in Kinshasa had an average of 4.2 children but reported wanting 3.6 children.9
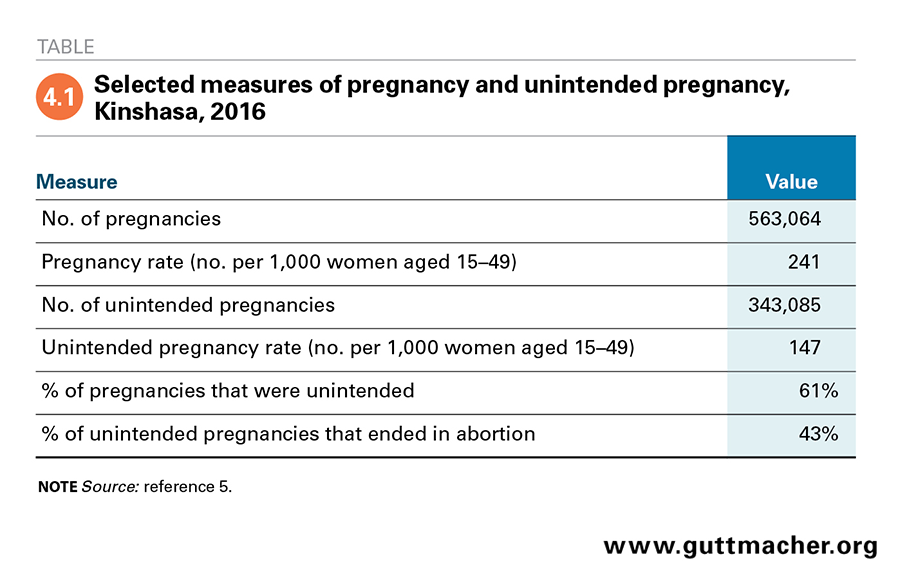
There were approximately 563,100 pregnancies in Kinshasa in 2016, according to estimates from the 2016 Kinshasa Abortion Study.5 Of these pregnancies, 61% were unintended (Table 4.1). These figures correspond to a pregnancy rate of 241 per 1,000 women aged 15–49 and an unintended pregnancy rate of 147 per 1,000 women aged 15–49.
Kinshasa’s unintended pregnancy rate of 147 per 1,000 women aged 15–49 is high compared with the global rate (62 per 1,000 women aged 15–44 in 2010–2014) and the rates for all developing countries (65) and Middle Africa (103).70 Across major cities in Sub-Saharan Africa, Kinshasa’s unintended pregnancy rate is higher than rates for same- or similar-aged women in Addis Ababa (123)34 and Kampala (132),35 and lower than the rate in Kigali (172).36
Characteristics of women having an abortion
The characteristics of women in Kinshasa who choose to end an unwanted or mistimed pregnancy are reported by only a handful of studies, most of which are relatively old. According to a 1984 study in Kinshasa of women presenting in university hospitals for "therapeutic abortion" or for complications related to abortion or miscarriage, the two groups of women most likely to have had an abortion were women younger than 20 who were unmarried, in school or poor, and who had had no more than two pregnancies; and women aged 20 and older who were married, educated and economically active.63 A 1990 survey of households in Kinshasa that explored women’s prior pregnancies, including those that were terminated, found that incidence of abortion rose with educational attainment, up to when women reached upper-level secondary schooling.21 Incidence of abortion was also higher among women employed in the "modern sector" than among their unemployed or self-employed peers and higher among unmarried women than among married women. Belonging to certain religious and ethnic groups was positively or negatively associated with having had an abortion, depending on the specific group. A 2003 household survey exploring contraceptive use in Kinshasa found age to be associated with having had an abortion: Women aged 15–19 and 45–49 were the age-groups most likely to report having terminated a pregnancy.24 A 2014 study of women presenting for emergency gynecologic and obstetric care found that abortion complications were twice as common among adolescent patients as among older patients.64
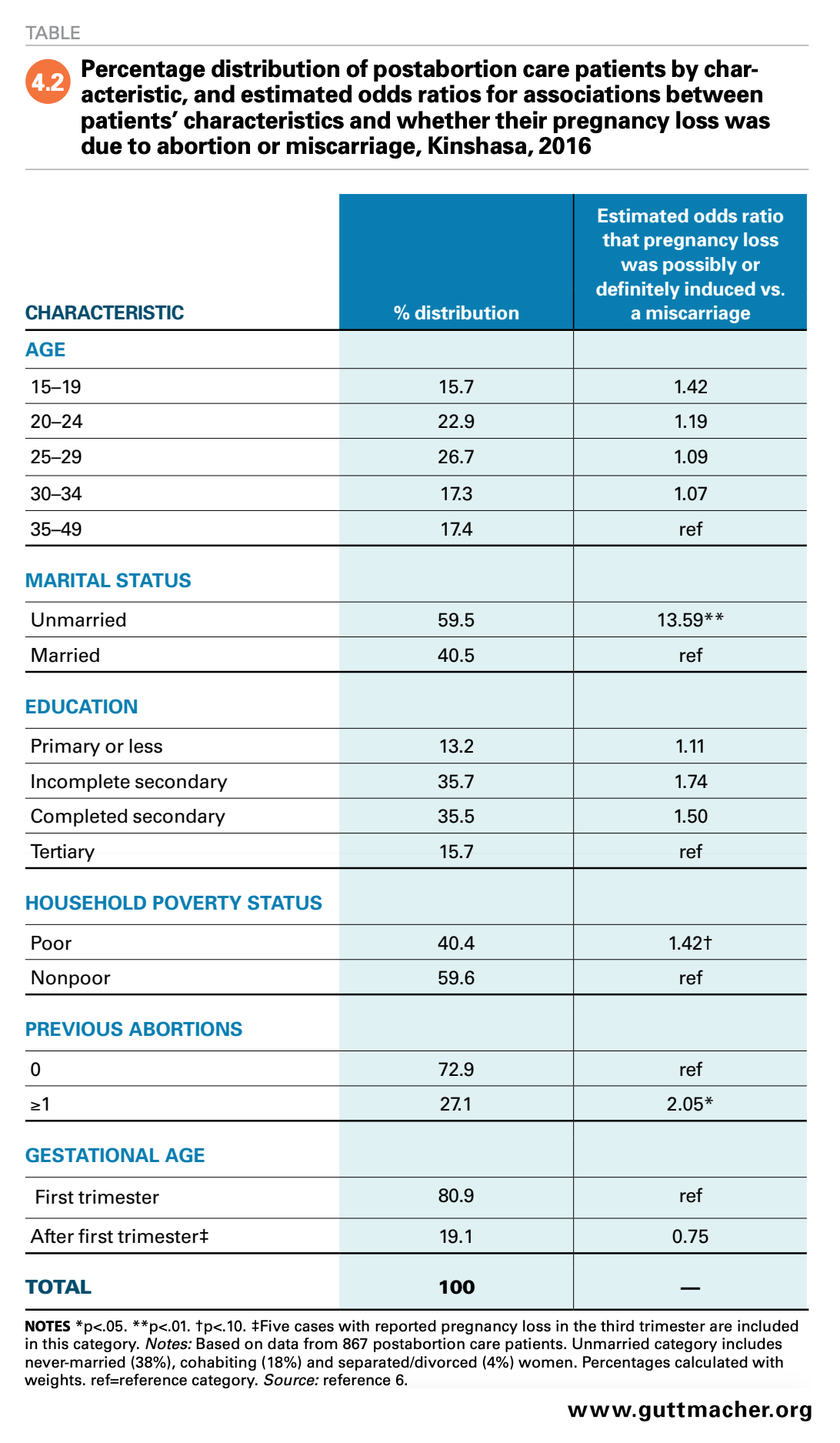
Focusing on women presenting for postabortion care in the 2016 Kinshasa Abortion Study’s Prospective Morbidity Study, the odds that women possibly or definitely had an abortion (rather than a miscarriage) were more than 13 times as high among unmarried women as among those who were married (Table 4.2).6 Past experience with abortion was also associated with having possibly or definitely having had an abortion: Women who had one or more prior abortions had double the odds of having postabortion care following an abortion (rather than a miscarriage), compared with women who reported no prior abortions. Finally, postabortion care patients from poor households had 42% higher odds of certainly or possibly having had an abortion, relative to nonpoor peers.
Contextualizing abortion incidence
The choice to terminate a pregnancy is, of course, not solely dependent on women’s characteristics but is also influenced by a wide range of factors, including the legal, social and cultural context in which that decision is made. Previous research has shown that whether and how often abortion occurs in a given country is largely unrelated to its legal status.71 Rather, legal status predicts whether abortions are more likely to occur under safe or unsafe conditions. In settings such as Kinshasa, where abortion is highly restricted by law, all women who choose to terminate a pregnancy are at risk of experiencing an unsafe abortion.59 This risk may be especially high for those who lack the means to seek out and pay for safe services.
Women’s status in society and their exposure to social harms also affect their need for and decision making around abortion. Because sexual activity and childbearing among unmarried women is stigmatized—particularly in traditional or conservative societies, like those found in much of the DRC—unmarried women are at increased risk for seeking clandestine abortion and thus for experiencing complications.6,39 Violence against women is also a particularly important issue in this regard. According to research from the eastern part of the country, where political violence persists, women who have experienced sexual violence are at increased risk for unsafe abortion due to stigma associated with being a victim of sexual violence, which can result in castigation within formal health care services, and elevated motivation to terminate the pregnancy resulting from sexual violence.39
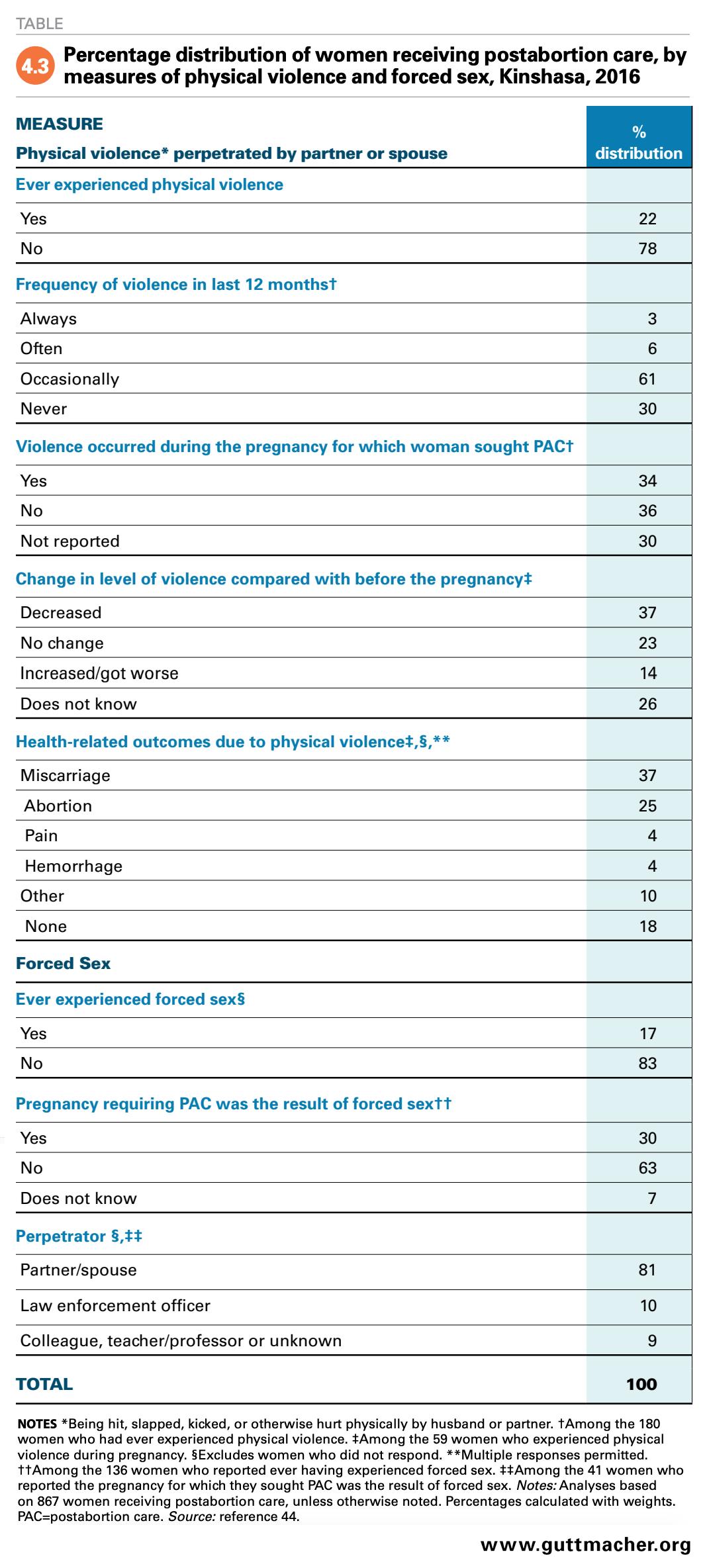
In Kinshasa, where the kind of armed conflict seen in the east of the DRC has been less prevalent, there is little information on the association of pregnancy and experiences of violence. However, the 2016 Kinshasa Abortion Study’s Prospective Morbidity Study asked women receiving postabortion care about their experiences with physical and sexual violence. More than one in five women (22%) reported ever having been hit, slapped, kicked or otherwise hurt physically by their husband or partner (Table 4.3).44 Among these women, more than one-third (34%) had experienced physical violence perpetrated by their partner during the pregnancy for which they were seeking postabortion care. In fact, 37% of women who experienced violence during their pregnancy indicated that the violence contributed to a miscarriage, and 25% indicated that it led to an unsafe abortion. In addition, 17% of postabortion care patients reported ever having experienced forced sex, and 30% of these women reported that the pregnancy for which they were seeking care resulted from this forced sex. The perpetrator in those cases was most often a partner or spouse (81%).
The findings on general experiences of violence in the 2016 Kinshasa Abortion Study are in line with data from the 2013–2014 DHS, which found 21% of women in the city experienced physical violence "sometimes or frequently" in the 12 months prior to the survey, and 16% of women had ever experienced sexual violence.9 This underscores the importance of understanding women’s risk for violence and the circumstances leading them to opt for an abortion.
Experts’ opinions on reducing unsafe abortion and its complications in the DRC
In the 2016 Kinshasa Abortion Study, the key informants interviewed for the Health Professionals Survey and respondents surveyed in the Health Facilities Survey were asked for their opinions on various aspects of the provision of abortion and postabortion care.
When asked the best ways to reduce unsafe abortion in the city and what measures should be prioritized, the vast majority (87%) of Health Professionals Survey key informants recommended improving information about and access to contraception, and nearly half recommended publicizing the health risks of unsafe abortion.42 The majority (87%) disagreed that the law criminalizing abortion should be enforced more strongly; rather, 73% of key informants thought the law should be liberalized.
Nearly all key informants felt that abortion should be legally allowed if the woman’s physical health is at risk.42 Some 64% of key informants thought abortion should be allowed in cases of severe fetal anomaly; 50% agreed with provision in cases of rape and 36% agreed with provision in cases of incest. Slightly fewer than a third (31%) thought abortion should be allowed if the pregnant woman is intellectually disabled or if her mental health is at risk (30%). Health Facilities Survey respondents’ views differed somewhat from those of the key informants. Four-fifths (81%) supported allowing legal abortion when the woman’s physical health is at risk, 54% thought abortion should be allowed in cases of severe fetal anomaly, while 36% thought it should be allowed for the purpose of preserving the woman’s mental health. A fifth of respondents thought that abortion should be allowed if the woman has an intellectual disability or if the pregnancy was the result of rape.72 Only 15% of health facility respondents thought that the abortion law should be changed to allow abortion under additional circumstances.
With respect to the provision of postabortion care, slightly more than half of the key informants (54%) thought that improving and developing infrastructure for such services would help reduce the consequences of unsafe abortion, and 45% of informants agreed that having a higher number of qualified providers would contribute to this goal.42 Among respondents to the Health Facilities Survey, 57% reported that services could be improved by strengthening technical capacity, 28% by greater availability of medication and supplies, 26% by improved and expanded infrastructure, and 15% by increasing the number of trained personnel.72 Only 7% of respondents reported that they consider provision in their facilities to be adequate.
Conclusions and Recommendations
In the face of great challenges, including more than two decades of armed conflict, the DRC’s recent progress on sexual and reproductive health is promising. The country’s commitment to legal reform that improves access to sexual and reproductive health services, and its recognition of the importance of delaying marriage, improving access to education and empowering women will likely contribute to long-term positive change.32
Even while steps are being taken to implement the Maputo Protocol and other recent policy reforms, many women in the DRC have an urgent need for sexual and reproductive health care, particularly contraceptive and postabortion care services. The 2016 Kinshasa Abortion Study provides up-to-date, actionable data highlighting current needs. Of the roughly 563,100 pregnancies occurring in the city in 2016, 61% were unintended, ultimately resulting in an estimated 146,700 abortions.5
Because of the highly restricted nature of abortion in the DRC, most abortions that occur in Kinshasa are unsafe. Many women experience complications, and a sizable share do not receive the medical care they require. As is true globally, the adverse health outcomes resulting from limited access to sexual and reproductive health services, including postabortion care services, in Kinshasa are inequitably borne by disadvantaged women, including those who are young and poor.
The costs of failing to meet women’s needs for sexual and reproductive health services are high, both economically and in terms of maternal mortality and morbidity. Women, families and society at large are negatively affected. Fortunately, complications associated with unsafe abortion are almost totally preventable, as are the majority of unintended pregnancies that end in abortion, and steps must be taken to prevent both, as well as to improve existing services.
Although no data are available on the health system costs of providing postabortion care in Kinshasa, based on data from other African country-level settings, they are likely significant. For example, in Nigeria, the annual health system costs of providing postabortion care in 2007 were estimated to be $19 million.73 Further, meeting all women’s needs for postabortion care would increase costs to the health system in Kinshasa beyond their current level. In Uganda, the total annual cost of providing postabortion care at documented levels in 2010 was estimated to be $13.9 million, and satisfying all need for such care would have increased that cost to $20.8 million per year.74 Likewise, in Rwanda, current care in 2012 was estimated at $1.7 million per year, and satisfying all need for such care would have increased costs to $2.5 million per year.75
Recommendations
The following are recommendations for meeting the DRC’s health and development goals pertaining to sexual and reproductive health, and for addressing the inequitable and adverse reproductive health outcomes in the country currently. Implementation of these recommendations could go a long way toward reducing unintended pregnancy and unsafe abortion in Kinshasa and at the national level.
Continue recent efforts to improve contraceptive access and uptake among women wanting to space or limit childbearing. There are many documented ways to increase access to and uptake of contraception and support continued use of contraception over time.76 However, improving service quality has been shown to be one of the most important factors for increasing contraceptive uptake.77–80 High-quality contraceptive service provision involves a range of factors, including ensuring that providers have needed skills and supportive, nonjudgmental attitudes, and establishing care that is responsive to the needs of particular populations, including young, poor, rural and unmarried women. Offering all women their choice among a range of methods is also critical: A study of Demographic and Health Survey data from African, Asian and Latin American countries estimated that for every additional contraceptive method that is affordable and consistently in stock at health facilities that women in need of contraception can easily access, the national contraceptive prevalence rate increases by 5–8 percentage points.81 Similarly, in a DRC study, the number of couple-years of protection provided by a health facility increased by almost eight for each additional contraceptive method they made available.82
Demand-generating interventions are also important for alerting women to the availability and benefits of contraceptives. Mass media campaigns, one-on-one education sessions and use of cash transfers have all been shown to influence uptake.76 In a 2010 study in Butembo, one of the largest cities in eastern DRC, teenage mothers had poor knowledge of traditional and modern family planning options, yet nearly one in three study respondents requested to be taught how to use methods.83
In addition to individual-level predictors of uptake, policymakers in the DRC must consider the influence of local and regional macroeconomic factors, conflicts and infrastructure (including transport routes) when striving to improve contraceptive access.84 The country is vast, and progress will be incremental. However, investment in expanding and improving contraceptive services will reduce the cost of postabortion care while also reducing costs associated with maternal and newborn health care—ultimately freeing up funds for further health systems investments.85,86
Transition to recommended methods for providing postabortion care. In Kinshasa, the postabortion care provided to women is not compliant with internationally established best practices. The World Health Organization recommends manual vacuum aspiration (MVA) for first-line management of incomplete abortion, and it recommends use of misoprostol if a trained provider is not available.87 Prophylactic antibiotics are recommended for all uncomplicated cases, and for pain relief, nonsteroidal anti-inflammatory drugs should be offered to all women and administered immediately if requested. The guidelines also strongly recommend providing contraceptive services to all postabortion care patients.
Bringing service provision in Kinshasa in line with international standards will require strengthening the capacity of the health system, at both primary and secondary referral levels. In the meantime, postabortion care services can be improved incrementally. Dilation and curettage requires highly skilled health professionals, sterilized equipment, an operating theater and significant patient care. Expenses to health facilities and patients could be minimized if less invasive, recommended uterine evacuation methods were used.88–90 Also, training nurses and midwives to safely provide both MVA and misoprostol for uncomplicated incomplete abortion would increase the pool of providers available to offer these recommended methods.91 Although oversight from doctors (and sometimes specialists) is required for managing complicated cases, such as those involving infection and hemorrhage, trained midlevel health professionals can provide initial management of such cases.
Improve access to postabortion care services. Bringing postabortion care services in line with international guidance would greatly improve quality of care. However, ensuring access to care also requires quality services that are affordable and offered in close proximity to those who need them.92 Women in Kinshasa may face fewer geographical barriers to access than women outside the capital; however, according to the 2016 Kinshasa Abortion Study, most postabortion care in Kinshasa is provided in private and NGO facilities, where services are likely more expensive than at public facilities. Even for women obtaining care in public facilities, there is evidence that under-the-table fees for services may be commonplace.93 Whether women go to private and NGO facilities or public facilities, they likely incur expenses, and, as has been shown elsewhere, women and their households may bear a sizable share of the direct costs of obtaining postabortion care.73 Women frequently pay out-of-pocket for some portion of abortion-related costs in countries where access to safe services is limited,73,74,94–96 and out-of-pocket costs are just one component of health service costs. Additional indirect costs may include lost productivity and wages, interference with children’s education, and deterioration in economic circumstances at the individual and household level.97,98
Address gender inequality and violence against women. Interventions addressing gender inequality and women’s roles in the DRC would reap broad benefits, as women are major contributors to the well-being and prosperity of their families and communities,99 provide vital income, and have a large influence on children’s health and educational attainment.97 Having ever experienced intimate partner violence is associated with a number of poor physical and mental health outcomes.100,101 In addition, survivors of sexual violence in the DRC report myriad health and psychosocial problems, including STIs and unwanted pregnancy.102 Taking steps to eliminate all forms of violence against women would go a long way toward improving women’s health, well-being and quality of life in Kinshasa and the DRC. Reducing gender disparities, supporting and empowering women, and addressing attitudes that devalue women have potential for great rewards, including improved sexual and reproductive health outcomes, a reduction in poverty and a better outlook for future generations.
Expand access to safe abortion by combatting stigma and implementing Maputo Protocol provisions. Changing the highly restrictive legal status of abortion would substantially improve health outcomes in Kinshasa by making abortion safer and more accessible. Women’s health advocates in the DRC have long worked toward legalization of abortion, including by publicly calling for decriminalization and recently pushing for publication of the Maputo Protocol.63,103 In the 2016 Kinshasa Abortion Study (which was fielded prior to publication of the protocol), substantial proportions of key informants and health facilities administrators were in support of liberalizing the country’s penal code, although they did not always agree on the conditions under which abortion should be allowed.
Globally, sociocultural opposition to abortion has been identified as a barrier that not only prevents women from seeking care but also prevents providers from offering it.104–107 Combatting the impact of abortion-related stigma will be integral to implementing the provisions of the Maputo Protocol. This will require sensitizing health care providers, communities, policymakers and other stakeholders. Values clarification and attitude transformation (VCAT) workshops may be a valuable resource, as these types of workshops engage participants "in a process of self-examination with the goal of transforming abortion-related attitudes and behaviors in a direction supportive of women seeking abortion."108 An assessment of pre- and postworkshop surveys from VCAT workshops in Asia, Africa and Latin America between 2006 and 2011 revealed improvements in participant knowledge, attitudes and intended behaviors related to abortion care; the largest impact was identified among workshop participants who had the least knowledge and the most negative attitudes about abortion at the start.
Evidence of the impact of liberalizing countries’ abortion laws in other settings may also help to convince local health care workers and policymakers of the value of expanding access under the protocol. In South Africa, the proportion of maternal mortality attributed to unsafe abortion in the country dropped by 91% in the four years following an expansion in the legal indications for abortion.109 That said, access to safe services does not occur overnight. Training and equipping health professionals to provide safe abortion services, and educating the population regarding access to services takes time. Improvements in postabortion care will continue to be needed, even as safe abortion services are expanded. Ethiopia changed its highly restrictive abortion law in 2005, and public education about abortion availability is still ongoing. An evaluation of changes after legal reform found that between 2008 and 2014, there was a more than 39% increase in the estimated annual number of women presenting for legal abortion.110 There were concurrent increases in the share of abortion procedures performed using medication abortion, the proportion of abortion care provided by midlevel health workers and the proportion of patients receiving postabortion contraception. At the same time, the country experienced a more than doubling of the estimated number of women presenting for postabortion care, potentially due to a combination of reduced stigma and increased access to postabortion care services.
Conduct more research on sexual and reproductive health, including on abortion among adolescents. Additional research would be beneficial in understanding the shortfalls of sexual and reproductive health policies, services and practices in the DRC. The DRC’s national sexual and reproductive health strategy includes establishing youth centers that offer youth- and adolescent-specific reproductive health services.111 Research on the sexual and reproductive health of adolescents—including on abortion among this age-group—would contribute to these efforts and is imperative to deepen the knowledge base pertaining to adolescents, especially as Kinshasa is a youthful city.
There is also a need for data on current costs to the DRC health care system of offering postabortion care. The likely high costs of postabortion care may provide extra incentive for policymakers to quicken the pace of implementing the Maputo Protocol.
Further, as implementation of the protocol proceeds in the country, research on the impact of steps taken to improve access to safe abortion services would be beneficial within and outside of the DRC. There are little or no data on adolescent access to or experiences of abortion in the DRC, and efforts to track increased access for young women and adolescents would help to fill this specific information gap.
Continuing progress
More than 30 years ago, researchers in the DRC posited that the costs of unsafe abortion in the country were high, and they called for improving access to contraception and liberalizing the country’s abortion law as two strategies for addressing the public health problem.63 Recommendations for the country are surprisingly similar today. There is a need to improve infrastructure and access to high-quality health services generally, but there is a particular need for will and commitment, both politically and socially, to invest in and improve sexual and reproductive health services. To address high levels of morbidity and mortality among women in the country, immediate attention is required. Steps should be taken to combat abortion-related stigma and to implement the Maputo Protocol as quickly and efficiently as possible. In addition, improvements to existing contraceptive and postabortion care services will contribute to attaining the Sustainable Development Goals, reducing unmet need for contraception and maternal mortality, as well as achieving other objectives.112
Recent developments in sexual and reproductive health policy in the DRC have created an opportunity to realize change that will benefit women, families, communities and, ultimately, the country as a whole. The momentum must be maintained if these benefits are to become a reality.
Footnotes
*All monetary amounts from the 2016 Kinshasa Abortion Study are reported in 2016 U.S. dollars.
†A new definition of abortion safety put forward in 2017 categorizes abortions into three categories: least safe, less safe and safe. Because the change in defintions happened after the 2016 Kinshasa Abortion Study was completed, our data refer to "unsafe" abortion, a designation that equates to the least safe and less safe categories combined.
‡Measured in disability-adjusted life years (DALYs), a measure designed to facilitate comparisons of the burdens of premature death and disability attributable to different causes across contexts. DALYs due to abortion complications are largely preventable.
References
1. Journal Officiel de la République Démocratique du Congo, Code Penal Congolais, Décret du 30 janvier 1940 tel que modifié et complété à ce jour, Mis à jour au 30 novembre 2004.
2. Government of the Democratic Republic of the Congo, Ordonnance 70-158 Du 30 Avril 1970 Déterminant Les Règles de La Déontologie Médicale, 70–158, 1970, https://abortion-policies.srhr.org/documents/countries/03-Democratic-Re….
3. Journal Officiel de la République Démocratique du Congo, Cabinet du Président de la République, Law No. 06/015 of 12 June 2006 Authorizing the Accession of the Democratic Republic of the Congo to the Protocol to the African Charter on Human and Peoples’ Rights on the Rights of Women in Africa, Law No. 06/015, 2006, http://www.journalofficiel.cd/respubrescente.php?id_jo=1369&lib_parutio….
4. Center for Human Rights, University of Pretoria, Maputo Protocol turns 15! A call for states to ratify and implement the Protocol- moving from rhetoric to action, 2018, http://www.chr.up.ac.za/wru-news/832-maputo-protocol-turns-15-a-call-fo….
5. Chae S et al., The incidence of induced abortion in Kinshasa, Democratic Republic of Congo, 2016, PLOS ONE, 2017, 12(10):e0184389, doi:10.1371/journal.pone.0184389.
6. Bankole A et al., The severity and management of complications among postabortion patients treated in Kinshasa health facilities, International Perspectives on Sexual and Reproductive Health, 2018, 44(1), doi:10.1363/44e5618.
7. Rutstein SO and Johnson K, The DHS wealth index, DHS Comparative Reports, Calverton, MD, USA: ORC Macro, 2004, No. 6.
8. Filmer D and Pritchett LH, Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India, Demography, 2001, 38(1):115–132.
9. Ministry of Monitoring, Planning and Implementation of the Modern Revolution (MMPIMR) and Ministry of Public Health (MPH), Enquête Démographique et de Santé en République Démocratique du Congo 2013–2014, Kinshasa: MMPIMR and MPH; and Rockville, MD, USA: ICF International, 2014, https://dhsprogram.com/publications/publication-FR300-DHS-Final-Reports….
10. Performance Monitoring and Accountability 2020, PMA2017/Kinshasa, DRC Round 6 Family Planning Brief, 2018, https://www.pma2020.org/sites/default/files/EN-DRC-Kinshasa-R6-FP-Brief….
11. United Nations Human Settlements Programme, Urbanization and Development: Emerging Futures World Cities Report 2016, Nairobi, Kenya: UN Habitat, 2016.
12. United Nations Population Division, World Urbanization Prospects: The 2014 Revision, New York: United Nations Population Division, 2015.
13. World Bank, Population estimates and projections: Democratic Republic of Congo, World Bank DataBank, 2019, https://databank.worldbank.org/Population-growth-rate-DRC/id/8a4029ee.
14. International Monetary Fund, Democratic Republic of the Congo: selected issues, IMF Country Report, 2015, No. 15/281, http://elibrary.imf.org/view/IMF002/22882-9781513590189/22882-978151359….
15. World Bank, Poverty headcount ratio at $1.90 a day (2011 PPP) (% of population), 2019, https://data.worldbank.org/indicator/SI.POV.DDAY?end=2012&locations=CD&….
16. United Nations Development Program, Human Development Indices and Indicators: 2018 Statistical Update: Congo (Democratic Republic of The), 2018, http://hdr.undp.org/sites/all/themes/hdr_theme/country-notes/COD.pdf.
17. Human Rights Watch, DR Congo: chronology, Human Rights Watch, 2009, https://www.hrw.org/news/2009/08/21/dr-congo-chronology.
18. Kwete D et al., Family planning in the Democratic Republic of the Congo: encouraging momentum, formidable challenges, Global Health: Science and Practice, 2018, 6(1):40–54, doi:10.9745/GHSP-D-17-00346.
19. Peterman A, Palermo T and Bredenkamp C, Estimates and determinants of sexual violence against women in the Democratic Republic of Congo, American Journal of Public Health, 2011, 101(6):1060–1067.
20. Hindin MJ, Kishor S and Ansara DL, Intimate partner violence among couples in 10 DHS countries: predictors and health outcomes, DHS Analytical Studies, Calverton, MD, USA: Macro International Inc., 2008, No. 18.
21. Shapiro D and Tambashe BO, The impact of women’s employment and education on contraceptive use and abortion in Kinshasa, Zaire, Studies in Family Planning, 1994, 25(2):96–110, doi:10.2307/2138087.
22. Lupwana K, Clandestine and risk abortions of female adolescents by self-medication in the outskirts of Kinshasa: vulnerability factors, paper presented at the Sixth African Population Conference, Ouagadougou, Burkina Faso, Dec. 5–9, 2011, https://uaps2011.princeton.edu/abstracts/110572.
23. Paluku LJ et al., Knowledge and attitude of schoolgirls about illegal abortions in Goma, Democratic Republic of Congo, African Journal of Primary Health Care & Family Medicine, 2010, 2(1), doi:10.4102/phcfm.v2i1.78.
24. Kayembe PK et al., Prevalence and determinants of the use of modern contraceptive methods in Kinshasa, Democratic Republic of Congo, Contraception, 2006, 74(5):400–406, doi:10.1016/j.contraception.2006.06.006.
25. World Bank, GDP per capita (current US$) Democratic Republic of Congo data, 2019, https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?end=2016&locations=….
26. World Bank, GINI index (World Bank estimate) data, 2019, https://data.worldbank.org/indicator/SI.POV.GINI?contextual=default&loc….
27. World Health Organization, The Abuja Declaration: Ten Years On, 2011, http://www.who.int/healthsystems/publications/abuja_declaration/en/.
28. USAID, Democratic Republic of the Congo—global health, 2019, https://www.usaid.gov/democratic-republic-congo/global-health.
29. World Health Organization (WHO) et al., Trends in Maternal Mortality: 1990 to 2015. Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division, Geneva: WHO, 2015, http://www.who.int/reproductivehealth/publications/monitoring/maternal-….
30. Democratic Republic of Congo Ministry of Public Health, Family Planning National Multisectoral Strategic Plan (2014–2020), 2014, http://ec2-54-210-230-186.compute-1.amazonaws.com/wp-content/uploads/20….
31. Family Planning 2020, New Country Commitments to FP2020: Benin, Democratic Republic of the Congo (DRC), Guinea, Mauritania, and Myanmar, 2013, https://www.familyplanning2020.org/sites/default/files/2013_11-14_New_C….
32. Gouvernement de la Republique Democratique du Congo, Engagements Family Planning 2020, London: FP2020, 2017, http://ec2-54-210-230-186.compute-1.amazonaws.com/wp-content/uploads/20….
33. Ishoso DK et al., Extent of induced abortions and occurrence of complications in Kinshasa, Democratic Republic of the Congo, Reproductive Health, 2019, 16(1), doi:10.1186/s12978-019-0727-4.
34. Moore AM et al., The estimated incidence of induced abortion in Ethiopia, 2014: changes in the provision of services since 2008, International Perspectives on Sexual and Reproductive Health, 2016, 42(3), doi:10.1363/42e1816.
35. Prada E et al., Incidence of induced abortion in Uganda, 2013: new estimates since 2003, PLOS ONE, 2016, 11(11):e0165812, doi:10.1371/journal.pone.0165812.
36. Basinga P et al., Abortion incidence and postabortion care in Rwanda, Studies in Family Planning, 2012, 43(1):11–20.
37. Mohamed SF et al., The estimated incidence of induced abortion in Kenya: a cross-sectional study, BMC Pregnancy and Childbirth, 2015, 15(185), doi:10.1186/s12884-015-0621-1.
38. Sedgh G et al., Estimates of the incidence of induced abortion and consequences of unsafe abortion in Senegal, International Perspectives on Sexual and Reproductive Health, 2015, 41(1):11–19, doi:10.1363/4101115.
39. Burkhardt G et al., Sexual violence-related pregnancies in eastern Democratic Republic of Congo: a qualitative analysis of access to pregnancy termination services, Conflict and Health, 2016, 10(1), doi:10.1186/s13031-016-0097-2.
40. Rouhani SA et al., A quantitative assessment of termination of sexual violence-related pregnancies in eastern Democratic Republic of Congo, Conflict and Health, 2016, 10(1), doi:10.1186/s13031-016-0073-x.
41. Sherris J et al., Misoprostol use in developing countries: results from a multicountry study, International Journal of Gynecology & Obstetrics, 2005, 88(1):76–81, doi:10.1016/j.ijgo.2004.09.006.
42. Special tabulations of data from the 2016 Kinshasa Health Professionals Survey, 2018.
43. WHO, Safe Abortion: Technical and Policy Guidance for Health Systems, Second Edition, 2012.
44. Special tabulations of data from the 2016 Kinshasa Prospective Morbidity Survey, 2018.
45. Johnson-Hanks J, The lesser shame: abortion among educated women in southern Cameroon, Social Science & Medicine, 2002, 55(8):1337–1349.
46. Boltanski L, La condition foetale: une sociologie de l’engendrement et de l’avortement, Paris: Gallimard Essai, 2004.
47. Théry I, Avortement, engendrement et singularisation des êtres humains, Annales Histoire, Sciences Sociales, 2006, 61(02):481–503, doi:10.1017/S0395264900001384.
48. Figà-Talamanca I et al., Illegal abortion: an attempt to assess its cost to the health services and its incidence in the community, International Journal of Health Services: Planning, Administration, Evaluation, 1986, 16(3):375–389, doi:10.2190/BJ4F-9KJN-MFAL-6X22.
49. Ganatra B et al., Global, regional, and subregional classification of abortions by safety, 2010–14: estimates from a Bayesian hierarchical model, Lancet, 2017, 390(10110):2372–2381, doi:10.1016/S0140-6736(17)31794-4.
50. Singh S et al., Abortion Worldwide 2017: Uneven Progress and Unequal Access, New York: Guttmacher Institute, 2018.
51. Darroch JE, Adding It Up: Investing in Contraception and Maternal and Newborn Health, 2017—Estimation Methodology, New York: Guttmacher Institute, 2018, supplementary table 36, https://www.guttmacher.org/report/adding-it-up-investing-in-contracepti….
52. Pande RP et al., Continuing with "…a heavy heart"—consequences of maternal death in rural Kenya, Reproductive Health, 2015, 12(S1), doi:10.1186/1742-4755-12-S1-S2.
53. Molla M et al., Impacts of maternal mortality on living children and families: a qualitative study from Butajira, Ethiopia, Reproductive Health, 2015, 12(S1), doi:10.1186/1742-4755-12-S1-S6.
54. Bazile J et al., Intergenerational impacts of maternal mortality: qualitative findings from rural Malawi, Reproductive Health, 2015, 12(S1), doi:10.1186/1742-4755-12-S1-S1.
55. Knight L and Yamin AE, "Without a mother": caregivers and community members’ views about the impacts of maternal mortality on families in KwaZulu-Natal, South Africa, Reproductive Health, 2015, 12(S1), doi:10.1186/1742-4755-12-S1-S5.
56. Kes A et al., The economic burden of maternal mortality on households: evidence from three sub-counties in rural western Kenya, Reproductive Health, 2015, 12(S1), doi:10.1186/1742-4755-12-S1-S3.
57. Kirigia JM et al., Indirect cost of maternal deaths in the WHO African Region in 2010, BMC Pregnancy and Childbirth, 2014, 14(1), doi:10.1186/1471-2393-14-299.
58. Family Care International (FCI) et al., A Price Too High to Bear: The Costs of Maternal Mortality to Families and Communities, New York: FCI; Washington, DC: International Council for Research on Women; and Nairobi, Kenya: KEMRI/CDC Research and Public Health Collaborative, 2014.
59. World Health Organization, Preventing unsafe abortion, 2018, http://www.who.int/news-room/fact-sheets/detail/preventing-unsafe-abort….
60. World Health Organization, Clinical Guidelines for Emergency Treatment of Abortion Complications, 1994, No. WHO/FHE/MSM/94.1, http://www.postabortioncare.org/sites/pac/files/WHO_Clinical_Management….
61. Singh S, Darroch JE and Ashford LS, Adding It Up: The Costs and Benefits of Investing in Sexual and Reproductive Health 2014, New York: Guttmacher Institute, 2014.
62. Guttmacher Institute, Postabortion care in Kinshasa, 2016, infographic, 2018, https://www.guttmacher.org/infographic/2018/postabortion-care-kinshasa-….
63. Tshibangu K et al., Avortement clandestin, problème de santé publique à Kinshasa (Zaïre), Journal de Gynecologie, Obstetrique et Biologie de la Reproduction, 1984, 13(7):759–763.
64. Ishoso DK, Tshefu AK and Coppieters Y, Analysis of induced abortion-related complications in women admitted to referral health facilities in Kinshasa, Democratic Republic of the Congo, PLOS ONE, 2018, 13(8):e0203186, doi:10.1371/journal.pone.0203186.
65. Grossman D et al., Surgical and medical second trimester abortion in South Africa: a cross-sectional study, BMC Health Services Research, 2011, 11(1), doi:10.1186/1472-6963-11-224.
66. Sedgh G et al., Abortion incidence between 1990 and 2014: global, regional, and subregional levels and trends, Lancet, 2016, 388(10041):258–267, doi:10.1016/S0140-6736(16)30380-4.
67. Kidman R, Palermo T and Bertrand J, Intimate partner violence, modern contraceptive use and conflict in the Democratic Republic of the Congo, Social Science & Medicine, 2015, 133:2–10, doi:10.1016/j.socscimed.2015.03.034.
68. Muanda MF et al., Barriers to modern contraceptive use in rural areas in DRC, Culture, Health & Sexuality, 2017, 19(9):1011–1023, doi:10.1080/13691058.2017.1286690.
69. Babazadeh S et al., Assessing the contraceptive supply environment in Kinshasa, DRC: trend data from PMA2020, Health Policy and Planning, 2018, 33(2):155–162, doi:10.1093/heapol/czx134.
70. Bearak J et al., Global, regional, and subregional trends in unintended pregnancy and its outcomes from 1990 to 2014: estimates from a Bayesian hierarchical model, Lancet Global Health, 2018, 6(4):e380–e389, doi:10.1016/S2214-109X(18)30029-9.
71. Sedgh G et al., Induced abortion: estimated rates and trends worldwide, Lancet, 2007, 370(9595):1338–1345, doi:10.1016/S0140-6736(07)61575-X.
72. Special tabulations of data from the 2016 Kinshasa Health Facilities Survey, 2018.
73. Bankole A et al., Estimating the cost of post-abortion care in Nigeria: a case study, in: Lule E, Singh S and Chowdhury S, eds., Fertility Regulation Behaviors and Their Costs: Contraception and Unintended Pregnancies in Africa and Eastern Europe & Central Asia, Washington, DC: World Bank, 2007, pp. 65–92.
74. Vlassoff M et al., The health system cost of post-abortion care in Uganda, Health Policy and Planning, 2014, 29(1):56–66, doi:10.1093/heapol/czs133.
75. Vlassoff M et al., The health system cost of post-abortion care in Rwanda, Health Policy and Planning, 2015, 30(2):223–233, doi:10.1093/heapol/czu006.
76. Mwaikambo L et al., What works in family planning interventions: a systematic review, Studies in Family Planning, 2011, 42(2):67–82, doi:10.1111/j.1728-4465.2011.00267.x.
77. Mensch B and Arends-Kuenning M, The impact of the quality of family planning services on contraceptive use in Peru, Studies in Family Planning, 1996, 27(2):59–75.
78. Arends-Kuenning M and Kessy FL, The impact of demand factors, quality of care and access to facilities on contraceptive use in Tanzania, Journal of Biosocial Science, 2007, 39:1–26.
79. Mroz TA et al., Quality, accessibility, and contraceptive use in rural Tanzania, Demography, 1999, 36(1):23–40.
80. Koenig M, Hossain M and Whitaker M, The influence of quality of care upon contraceptive use in rural Bangladesh, Studies in Family Planning, 1997, 28(4):278–289.
81. Futures Institute, The impact of stock-outs on the use of modern contraception, paper presented at the annual meeting of the International Conference on Family Planning, Addis Ababa, Ethiopia, Nov. 12–13, 2013.
82. Kayembe P et al., Family planning supply environment in Kinshasa, DRC: survey findings and their value in advancing family planning programming, Global Health: Science and Practice, 2015, 3(4):630–645, doi:10.9745/GHSP-D-15-00298.
83. Mathe JK, Kasonia KK and Maliro AK, Barriers to adoption of family planning among women in eastern Democratic Republic of Congo, African Journal of Reproductive Health, 2011, 15(1):69–77.
84. Kandala NB et al., Disparities in modern contraception use among women in the Democratic Republic of the Congo: a cross-sectional spatial analysis of provincial variations based on provincial variations based on household survey data, Journal of Biosocial Science, 2015, 47(3):345–362, doi:10.1017/S0021932014000212.
85. Johnston HB, Gallo MF and Benson J, Reducing the costs to health systems of unsafe abortion: a comparison of four strategies, Journal of Family Planning and Reproductive Health Care, 2007, 33(4):250–257, doi:10.1783/147118907782101751.
86. Guttmacher Institute, Adding it up: investing in contraception and maternal and newborn health in Africa, Fact Sheet, 2017, https://www.guttmacher.org/sites/default/files/factsheet/adding-it-up-c….
87. WHO, Clinical Practice Handbook for Safe Abortion, Geneva: WHO, 2014.
88. American College of Obstetricians and Gynecologists Committee on International Affairs, ACOG committee opinion, 2009, No. 427, https://www.acog.org/-/media/Committee-Opinions/Committee-on-Internatio….
89. Koontz SL et al., Treating incomplete abortion in El Salvador: cost savings with manual vacuum aspiration, Contraception, 2003, 68(5):345–351.
90. You JHS and Chung TKH, Expectant, medical or surgical treatment for spontaneous abortion in first trimester of pregnancy: a cost analysis, Human Reproduction, 2005, 20(10):2873–2878, doi:10.1093/humrep/dei163.
91. WHO, Health Worker Roles in Providing Safe Abortion Care and Post-Abortion Contraception, Geneva: WHO, 2015.
92. Evans DB, Hsu J and Boerma T, Universal health coverage and universal access, Bulletin of the World Health Organization, 2013, 91(8):546-546A, doi:10.2471/BLT.13.125450.
93. Bertone MP, Lurton G and Mutombo PB, Investigating the remuneration of health workers in the DR Congo: implications for the health workforce and the health system in a fragile setting, Health Policy and Planning, 2016, 31(9):1143–1151, doi:10.1093/heapol/czv131.
94. Lince-Deroche N et al., Accessing medical and surgical first-trimester abortion services: women’s experiences and costs from an operations research study in KwaZulu-Natal Province, South Africa, Contraception, 2017, 96(2):72–80, doi:10.1016/j.contraception.2017.03.013.
95. Lince-Deroche N et al., The costs of accessing abortion in South Africa: women’s costs associated with second-trimester abortion services in Western Cape Province, Contraception, 2015, 92(4):339–344, doi:10.1016/j.contraception.2015.06.029.
96. Vlassoff M et al., The health system cost of post-abortion care in Ethiopia, International Journal Gynaecology Obstetrics, 2012, 118(Suppl. 2):S127–S133, doi:10.1016/S0020-7292(12)60011-3.
97. Sundaram A et al., Documenting the individual- and household-level cost of unsafe abortion in Uganda, International Perspectives on Sexual and Reproductive Health, 2013, 39(04):174–184, doi:10.1363/3917413.
98. Vlassoff M et al., Estimates of health care system costs of unsafe abortion in Africa and Latin America, International Perspectives on Sexual and Reproductive Health, 2009, 35(3):114–121, doi:10.1363/ipsrh.35.114.09.
99. World Bank, Women: The Future of Africa, Washington, DC: World Bank, 2018.
100. Ellsberg M et al., Intimate partner violence and women’s physical and mental health in the WHO multi-country study on women’s health and domestic violence: an observational study, Lancet, 2008, 371(9619):1165–1172, doi:10.1016/S0140-6736(08)60522-X.
101. Gibbs A, Dunkle K and Jewkes R, Emotional and economic intimate partner violence as key drivers of depression and suicidal ideation: a cross-sectional study among young women in informal settlements in South Africa, PLOS ONE, 2018, 13(4):e0194885, doi:10.1371/journal.pone.0194885.
102. Bartels S et al., Surviving sexual violence in eastern Democratic Republic of Congo, Journal of International Women’s Studies, 2010, 11(4):37–49.
103. Kalonda JCO, Sexual violence in Congo-Kinshasa: necessity of decriminalizing abortion, Revue médicale de Bruxelles, 2011, 33:482–486.
104. Culwell KR and Hurwitz M, Addressing barriers to safe abortion, International Journal of Gynecology & Obstetrics, 2013, 121(S1):S16–S19, doi:10.1016/j.ijgo.2013.02.003.
105. Rehnström Loi U et al., Health care providers’ perceptions of and attitudes towards induced abortions in sub-Saharan Africa and Southeast Asia: a systematic literature review of qualitative and quantitative data, BMC Public Health, 2015, 15(1):139, doi:10.1186/s12889-015-1502-2.
106. Payne CM et al., Why women are dying from unsafe abortion: narratives of Ghanaian abortion providers, African Journal of Reproductive Health, 2013, 17(2):118–128.
107. Mohamed D, Diamond-Smith N and Njunguru J, Stigma and agency: exploring young Kenyan women’s experiences with abortion stigma and individual agency, Reproductive Health Matters, 2018, 26(52):128–137, doi:10.1080/09688080.2018.1492285.
108. Turner KL et al., Values clarification workshops to improve abortion knowledge, attitudes and intentions: a pre-post assessment in 12 countries, Reproductive Health, 2018, 15(1):40, doi:10.1186/s12978-018-0480-0.
109. Jewkes R and Rees H, Dramatic decline in abortion mortality due to the Choice on Termination of Pregnancy Act, South African Medical Journal, 2005, 95(4):250–250.
110. Gebrehiwot Y et al., Changes in morbidity and abortion care in Ethiopia after legal reform: national results from 2008 and 2014, International Perspectives on Sexual and Reproductive Health, 2016, 42(3):121–130, doi:10.1363/42e1916.
111. Evidence to Action, Government of DRC announces creation of first national platform for engaging Congolese youth in AYSRH decision-making, press release, 2017, https://www.e2aproject.org/news-item/government-drc-announces-creation-….
112. United Nations, Sustainable Development Goals Knowledge Platform, Health and population, no date, https://sustainabledevelopment.un.org/topics/healthandpopulation.
Suggested Citation
Lince-Deroche N et al., Unintended Pregnancy and Abortion in Kinshasa, Democratic Republic of Congo: Challenges and Progress, New York: Guttmacher Institute, 2019, https://www.guttmacher.org/report/unintended-pregnancy-abortion-in-Kins….
Acknowledgments
This report was written by Naomi Lince-Deroche, Nakeisha Blades, Patrice Williams, Jesse Philbin and Akinrinola Bankole of the Guttmacher Institute; Patrick Kayembe and Crispin Mabika of the University of Kinshasa; and Susan London, independent consultant. It was edited by Haley Ball, Guttmacher Institute.
The authors would like to thank the following current and former Guttmacher colleagues for their contributions: Sophia Chae, who served as co–principal investigator of the research; Ann Biddlecom, Alanna Galati, Lisa Remez, Colette Rose, Sophia Sadinsky, Susheela Singh and Elizabeth Sully, for reviewing the report during its development; and Lorraine Kwok, for research assistance.
The authors are also grateful for the feedback and advice offered by the following external reviewers: Jane Bertrand, Tulane School of Public Health and Tropical Medicine; Jacques Emina, University of Kinshasa; Kate Gilles and Jerry Parks, Population Reference Bureau; and Françoise Mukuku, “Si Jeunesse Savait.”
We also appreciate the input of our advisory board members: Nguma Aloïs, Department of Gynecology and Obstetrics, University of Kinshasa; Brigitte Kini, World Health Organization; Lombeya Lisomba and Guy Mukumpuri, National Program on Reproductive Health, Ministry of Health (MoH), Democratic Republic of Congo (DRC); Alphonse Matondo, United Nations Population Fund; Moïse Mbile and Mbadu Muanda, National Program on Youth Health, MoH, DRC; and Lisa Mahoya and Kalume Tutu, MoH, DRC.
Data for this report are drawn from work conducted in 2016 in Kinshasa, DRC. The authors would like to acknowledge Denise Ngondo, of the University of Kinshasa School of Public Health, and Barthelemy Kalambayi, Francis Loka, Isaac Mukadi, Basile Tambashe and Guy Tshomba—all of the University of Kinshasa Department of Population and Development Science, for their contributions to the administration, planning and data collection for this work. Finally, we are grateful for contributions made by the survey interviewers, supervisors and survey respondents who participated in this work.
This report was made possible by grants from the David and Lucile Packard Foundation, the Swedish International Development Cooperation Agency, the Dutch Ministry of Foreign Affairs and the Norwegian Agency for Development Cooperation, and by UK Aid from the UK Government. The findings and conclusions in this report are those of the authors and do not necessarily reflect the positions and policies of the donors. The Guttmacher Institute gratefully acknowledges the unrestricted funding it receives from many individuals and foundations—including major grants from the William and Flora Hewlett Foundation and the David and Lucile Packard Foundation—which undergirds all of the Institute’s work.
Additional Downloads
Read More
The Severity and Management of Complications Among Postabortion Patients Treated in Kinshasa Health Facilities
Topic
Geography