This fact sheet summarizes the findings of a study titled Unintended Pregnancy and Abortion in India, which provides the first comprehensive estimates of the incidence of abortion and unintended pregnancy and of the provision of induced abortion and postabortion services in Assam, Bihar, Gujarat, Madhya Pradesh, Uttar Pradesh and Tamil Nadu.
Incidence of abortion and unintended pregnancy
- Induced abortion has been legal in India on a broad range of grounds since the Medical Termination of Pregnancy Act was passed in 1971. Abortion is permitted up to 20 weeks’ gestation when it is necessary to save a woman’s life or protect her physical or mental health, and in cases of economic or social necessity, rape, contraceptive failure among married couples and fetal anomaly.
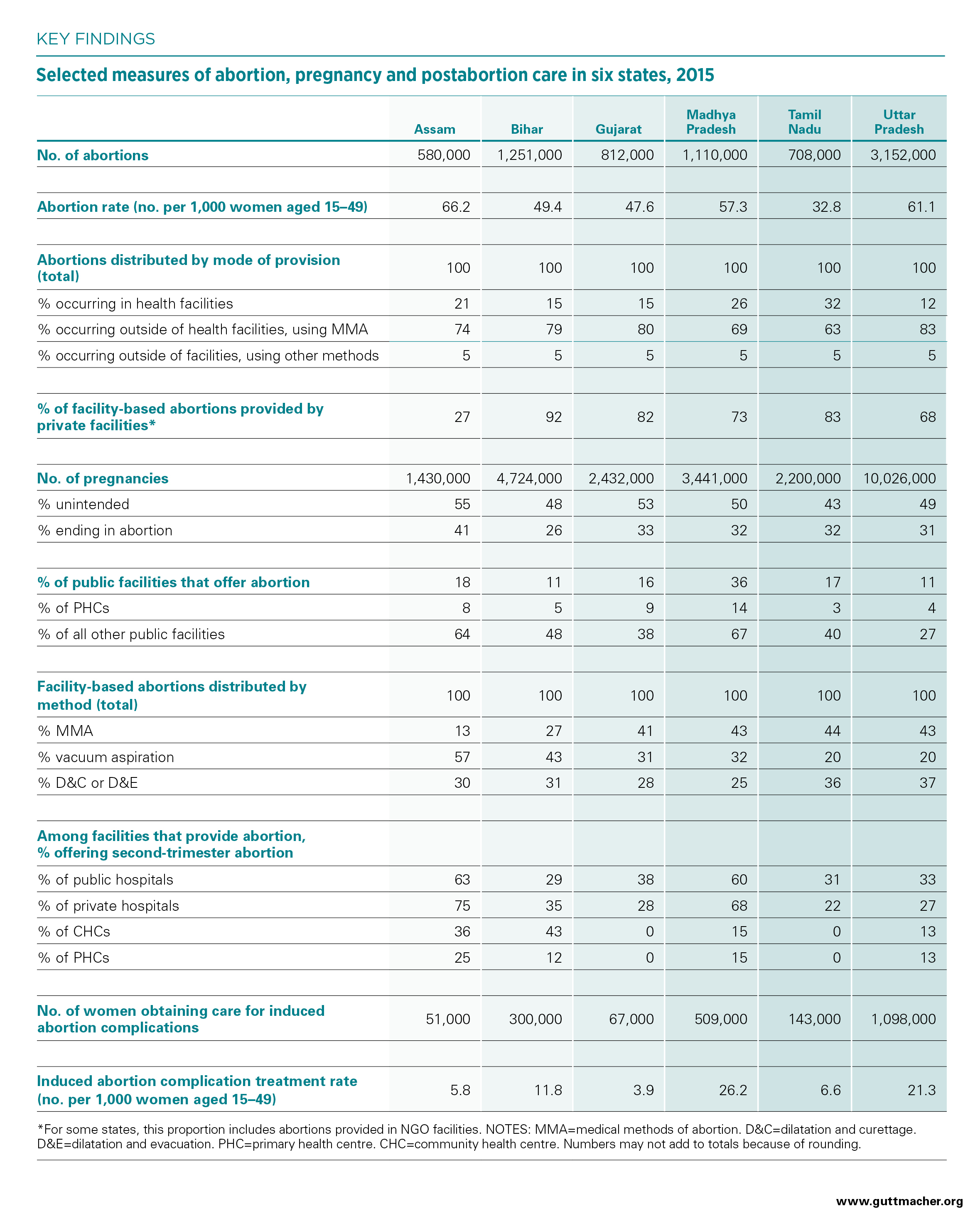
- The total number of abortions occurring in each of the six study states ranges widely (see table), and the magnitude of that number is largely dependent on population size. The abortion rate (the number of pregnancy terminations per 1,000 women aged 15–49) provides a means of comparing each of the study states directly. Abortion rates in the six states fall between 32.8 (in Tamil Nadu) and 66.2 (in Assam).
- Only a minority of the abortions occurring annually in each state are provided in health facilities. Facility-based abortions are done using either a surgical method, such as vacuum aspiration, dilatation and curettage (D&C) and dilatation and evacuation (D&E), or medical methods of abortion (MMA).*
- The majority of abortions in the six states (63–83%) are done using MMA obtained in settings other than health facilities, including from chemists and other informal vendors. Five percent of abortions in each state are performed outside of health facilities using other, typically unsafe methods.
- Except in Assam, the majority of facility-based abortions in the six states are provided in the private sector. Limitations on public-sector services are likely to have a disproportionately negative effect on poor and rural women.
- The number of abortions occurring annually in each state allows for estimation of the total number of pregnancies, which is the sum of births, miscarriages (including stillbirths) and induced abortions. Annual incidence of pregnancy ranges from 1.4 million in Assam to 10.0 million in Uttar Pradesh.
- Roughly half of all pregnancies are unintended, and 26–41% of all pregnancies end in abortion.
Provision of abortion in health facilities
- In five of the study states, more than three-quarters of facilities that provide induced abortion are private (hospitals, nursing and maternity homes, and clinics); in Assam, the slight majority are public.
- A minority of public facilities across all the study states offer abortion. Among PHCs, which are the most numerous type of public facility and which also tend to be small and underresourced, abortion provision is rare. Provision is higher among larger public facilities (hospitals, CHCs and other urban facilities), but it is far from universal; among these larger facilities combined, 27–67% across the six states offer the service.
- Among facilities that provide abortion, the majority offer both MMA and surgical terminations. Frequent use of D&C and D&E (for 25–37% of all facility-based abortions across the six states) indicates that facilities may be using methods that are outdated or are more invasive than necessary.
- In both the public and private sectors, many facilities that offer abortion do not provide it beyond certain gestational ages that are well below the 20-week legal limit. Among facilities that offer abortion, the majority of CHCs and PHCs—and many public and private hospitals—provide it only during the first trimester.
- Most facilities that offer abortion turn away one or more women per year seeking to terminate a pregnancy. Among these facilities, substantial proportions report reasons for doing so that may reflect provider bias or misinformation.
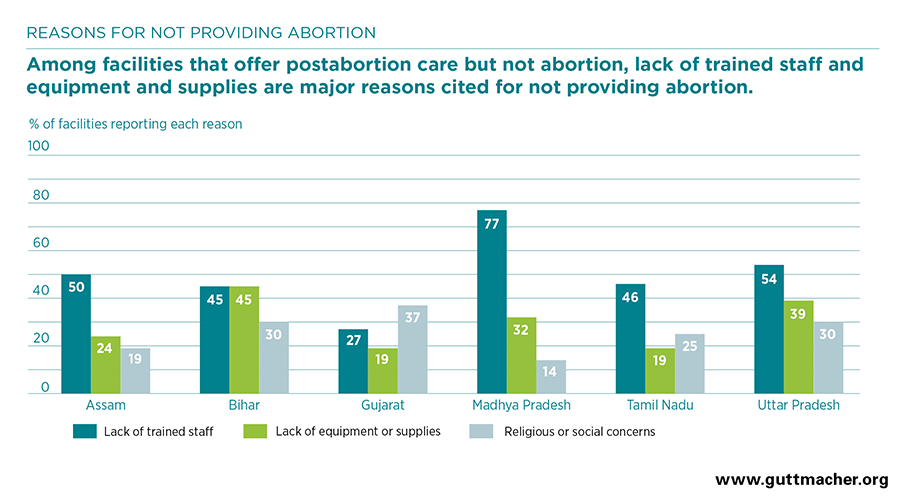
- Among public and private facilities that offer postabortion care but not abortion, lack of trained providers and lack of equipment or supplies are cited as major reasons for not providing abortion (see figure). Lack of registration to provide abortion is also a major barrier to provision among private facilities. Facility respondents suggest that stigma and cost are some of the major barriers preventing women from seeking out and obtaining an abortion.
- Almost all facilities that provide abortion-related services in the six study states report offering contraception after an abortion or postabortion care, but the majority provide only some components of comprehensive contraceptive care.
Postabortion care
- In the six study states, the number of women seeking care for complications of induced abortion ranges from 51,000 in Assam to 1,098,000 in Uttar Pradesh.
- The annual treatment rate, or the number of women treated for such complications per 1,000 women aged 15–49, varies from 3.9 in Gujarat to 26.2 in Madhya Pradesh.
- The majority of women receiving postabortion care are treated for relatively minor complications, such as incomplete abortion from MMA or prolonged or abnormal bleeding. However, many women in these categories are likely to have sought care unnecessarily because they mistook the normal process of MMA for a complication.
- An important minority of postabortion care patients across the six states experience one or more severe complications, such as infection (4–16%), physical injury (2–9%), sepsis (3–7%) or shock (1–4%). These complications are most likely the result of abortions that occur in nonfacility settings and are done using methods other than MMA.
- Generally, more facilities provide postabortion care than provide abortion. However, gaps in provision remain, and the reasons facilities cite for not providing postabortion care are similar to the reasons for not providing abortion.
Recommendations
- Improve access to facility-based abortion services, especially in underserved rural areas, by ensuring that all public-sector facilities have adequate equipment and supplies, including MMA drugs. In particular, increase PHCs’ capacity to provide abortion-related care, and streamline the process for registering private facilities to offer abortion.
- Offer MMA training for current and new providers, and increase the pool of approved providers by allowing nurses, auxiliary nurse midwives and practitioners trained in Indian systems of medicine to provide MMA and postabortion care.
- Ensure high-quality abortion care by training providers in current abortion techniques, best practices, legal criteria for abortion and nonjudgmental service provision.
- Use community-based health workers and public health campaigns to educate women about the availability of safe, legal abortion services in facilities, and inform them on the correct use of MMA.
- Ensure that high-quality, voluntary contraceptive services are available to all women, including those receiving abortion and postabortion care. Services should include provision of a wide range of methods and counseling on consistent and correct use.