- Research in four states—Arizona, Iowa, New Jersey and Wisconsin—that have varying sexual and reproductive health policies illustrates that restrictions appearing to target one type of reproductive health care have ripple effects on all aspects of reproductive care, including abortion and contraception.
- Research on the Trump administration’s 2019 Title X Final Rule, also known as the “domestic gag rule,” and related state polices provides evidence that policies seemingly aimed only at abortion can negatively impact health care systems and provider delivery of sexual and reproductive health care, as well as patients’ experiences of person-centered care and reproductive autonomy.
- Living in a state where the policies are generally protective of sexual and reproductive health care does not necessarily insulate individuals from the impact of restrictive federal policies. For example, the number of clinics in the Title X network and the number of people served by those clinics declined in New Jersey after the domestic gag rule took effect, similar to declines seen in states with more restrictive policies, such as Iowa and Wisconsin.
- The 2019 Title X Final Rule negatively impacted both clinics that chose to stay in and those that left the Title X network, limiting their services and the provision of person-centered care beyond what was dictated by the policy.
- Policy restrictions trickle down to impact individuals' experiences with care. For example, diminished access to high-quality, more affordable and more comprehensive sexual and reproductive health care resulted in some patients shifting their contraceptive use to a contraceptive method that they preferred less.
- Policy restrictions on sexual and reproductive health care compound existing inequities. Federal and state policies should fully fund Title X, ensure comprehensive coverage of all contraceptive options, and remove restrictions that silo abortion to promote reproductive autonomy and person-centered care.
Any Restrictions on Reproductive Health Care Harm Reproductive Autonomy: Evidence from Four States
Author(s)
Rachel Easter, Amy Friedrich-Karnik and Megan L. KavanaughReproductive rights are under attack. Will you help us fight back with facts?
Key Points
Background
It has been more than a year and a half since the Supreme Court decided Dobbs v. Jackson Women’s Health Organization, overturning Roe v. Wade and opening the floodgates for increasingly harsh attacks on abortion access. The Dobbs decision itself has had a devastating impact, but the decision was preceded by years of attacks on sexual and reproductive health care that were carried out in statehouses and at the federal level, most notably by the Trump administration. As the compounding impact of those policies was coming into focus, the COVID-19 pandemic struck, devastating public health infrastructure and deepening inequities in access to basic health care, housing, food and economic security.
Policymakers continue to grapple with the fallout of these historic, overlapping and continuing crises. Findings from the Reproductive Health Impact Study (RHIS)—a multiyear, multistate research initiative designed to comprehensively document and monitor the effects of federal and state policy changes on publicly funded sexual and reproductive health care, such as Title X, and the people who rely on it—can help clarify the impact of these changes and help policymakers craft solutions.
The research illustrates clearly that restrictions that may seem to target one type of reproductive health care have ripple effects on all aspects of reproductive health care, from abortion and contraception to pregnancy care. Moreover, these policies have a disproportionate impact on Black people and other people of color, LGBTQ+ individuals and people with low incomes, entrenching existing inequities and stymieing racial, gender and economic justice.1 As a result, policymakers must address sexual and reproductive health broadly, starting with the understanding that recent policies have created a crisis for people’s reproductive autonomy.
The Guttmacher Institute launched the RHIS after the 2016 election, in anticipation of federal and state efforts to change funding streams and service delivery for sexual and reproductive health care. The study focused on Arizona, Iowa and Wisconsin—states where a variety of policy restrictions on family planning services were expected—as well as New Jersey, which served as a comparison state because it is generally protective of reproductive health programs. The study has been tracking access to services and sexual and reproductive health outcomes from 2017 to 2024 to illuminate the impact of policy restrictions at multiple levels of health care. In doing so, RHIS has created a robust set of scientifically innovative findings that highlight the distinct but inextricably linked impact of these restrictions at the systems, health care provider and patient levels, all of which have implications for undermining people’s reproductive autonomy.
Key Definitions
The frameworks of reproductive autonomy and sexual and reproductive health equity stem from the reproductive justice movement, pioneered by Black women and other people of color.2,3 Similar to the framework of reproductive justice, these concepts were developed as part of long-standing efforts to improve access to reproductive health care for Black people and other people of color, as well as individuals with low incomes. These frameworks recognize that all forms of sexual and reproductive health care are inextricably linked, and that restrictions on any type of care negatively affect the provision of person-centered care and patients’ reproductive autonomy.
Reproductive autonomy is defined as having the power to decide about and control matters associated with contraceptive use, pregnancy and childbearing.4 This includes the power of every person to decide whether and when to be sexually active and to use contraceptive, abortion and pregnancy care, and how and when to access these types of care. Reproductive autonomy includes the ability to communicate, make decisions and counter coercion.5
Person-centered care is similar to patient-centered care, which is defined by the Institute of Medicine as “providing care that is respectful of, and responsive to, individual patient preferences, needs, and values and ensuring that patient values guide all clinical decisions.”6 Person-centered care recognizes that individuals often receive essential reproductive health care outside of the traditional provider-patient context. It is essential to reproductive autonomy, especially for communities long subject to reproductive oppression in this country: Black people and other people of color, young people, people with low incomes, undocumented immigrants and incarcerated individuals.
Sexual and reproductive health equity means that “all people, across the range of age, gender, race, and other intersectional identities, have what they need to attain their highest level of sexual and reproductive health.”7 Equitable access to the full range of sexual and reproductive health care must be supported by government policy and health care systems and structures that account for and seek to address inequities driven by racism, sexism and economic injustice, and center those most harmed. To achieve sexual and reproductive health equity, systems must equip individuals with the decision-making power to achieve their social, personal, financial, and sexual and reproductive health goals.7
How Policy Restrictions Impact Health Care Systems
Policy restrictions on sexual and reproductive health care negatively impact the health care systems in which these services are provided, resulting in less access to care and fewer people served.
The provision of health care in the United States is complex and expensive. The web of insurance coverage, public financing, differing care models and more is challenging for many providers and patients to navigate successfully. Further, the provision of reproductive health care is siloed and often stigmatized in the United States, and providers and facilities must overcome barriers and cost restrictions to provide patients with necessary care. Whether these barriers come in the form of bans on abortion care, restrictions on how to educate and inform patients of their options, or other policies that dictate the provision of sexual and reproductive health care, they can create hurdles that force providers to stop offering certain services or to permanently close facilities. Often, these facilities are essential health care providers in a community, offering all forms of reproductive—and primary—health care services, information and referrals.
The widespread detrimental effect that a policy can have was made evident after the Trump administration finalized a rule in 2019 that was seemingly about abortion, but targeted the Title X program, the nation’s publicly funded family planning program. The new policy, known as the 2019 Final Rule or “domestic gag rule,” prohibited abortion referrals; mandated that all pregnant patients receive referrals to prenatal care; required Title X grant recipients to be physically and financially separated from any abortion-related activities, including referrals and counseling; and redefined “family planning” to include abstinence, adoption and fertility awareness–based methods.
The disruptions caused by the 2019 Final Rule forced many Title X clinics to make a difficult decision: Stop providing all abortion services, including referrals, or leave the Title X program to be able to provide a full range of reproductive health care, including abortion referrals and care. The COVID-19 pandemic compounded the effects of the rule. Together, these two events resulted in the loss of 981 health care centers from the Title X network and an estimated 2.4 million fewer patients being served through the Title X program in 2020 as compared with 2018, a 61% drop that resulted in only 1.5 million people receiving Title X-supported services in 2020. Nearly two-thirds (63%) of that decrease in patients is attributed to the Final Rule and 37% to the impact of the COVID-19 pandemic.8,9
Data from the RHIS reveal that the number of Title X–funded clinics declined between 2018 and 2020, both in states with policies that are generally protective of sexual and reproductive health care, such as New Jersey, and states considered more hostile to this type of care, such as Wisconsin and Iowa.
In Wisconsin, the number of Title X–funded family planning clinics fell from 59 in 2018 to 39 clinics in 2020, and the number of Title X–funded family planning patients dropped from 40,162 to just 6,830 (Table 1). In Iowa, the number of Title X clinics declined from 43 to 38 and patients fell from 28,944 to 15,081 between 2018 and 2020. In New Jersey, the number of Title X clinics declined from 48 to 36 and the number of patients dropped from 96,294 in 2018 to 26,236 in 2020. In contrast, clinic numbers increased from 29 to 44 in Arizona during this time period but, as these sites were not ones that served large proportions of family planning patients, overall patient numbers still decreased from 29,319 to 12,287.
TABLE 1. Number and percentage change of Title X–funded clinics and patients served in 2018 and 2020
| ARIZONA | IOWA | ||||||
| 2018 | 2020 | % change | 2018 | 2020 | % change | ||
| Clinics | 29 | 44 | 52 | 43 | 38 | –12 | |
| Patients | 29,319 | 12,287 | –58 | 28,944 | 15,081 | –48 | |
| NEW JERSEY | WISCONSIN | ||||||
| 2018 | 2020 | % change | 2018 | 2020 | % change | ||
| Clinics | 48 | 36 | –25 | 59 | 39 | –34 | |
| Patients | 96,294 | 26,236 | –73 | 40,162 | 6,830 | –83 | |
In a few years, the Trump administration’s Title X rule had a devastating impact on the safety-net system of sexual and reproductive health care, which was established in 1970 with an explicit goal of reducing economic inequities in access to contraception.10 The impact was particularly acute in communities of color that, because of structural racism and decades of discrimination within the health care system, disproportionately rely on and are served by safety-net programs such as Title X. For example, while 13% of the US population is Black or African American,11 26% of Title X clients in 2020 identified as Black or African American; similarly, while 19% of the US population is Hispanic or Latino, more than one-third (35%) of Title X clients identified as Hispanic or Latino. More than 40% of immigrant women who accessed contraceptives did so at a safety-net family provider such as a Title X clinic.12
How Restrictions Impact Providers and Provision of Services
Policy restrictions on sexual and reproductive health care often force providers to overcome compounding hurdles to provide individuals with necessary sexual and reproductive health care. These hurdles can include everything from a clinic’s lack of financial stability to gag orders to outright bans on certain types of care. RHIS research documenting the fallout after the 2019 Title X rule illustrates the impact of this type of restriction on providers.
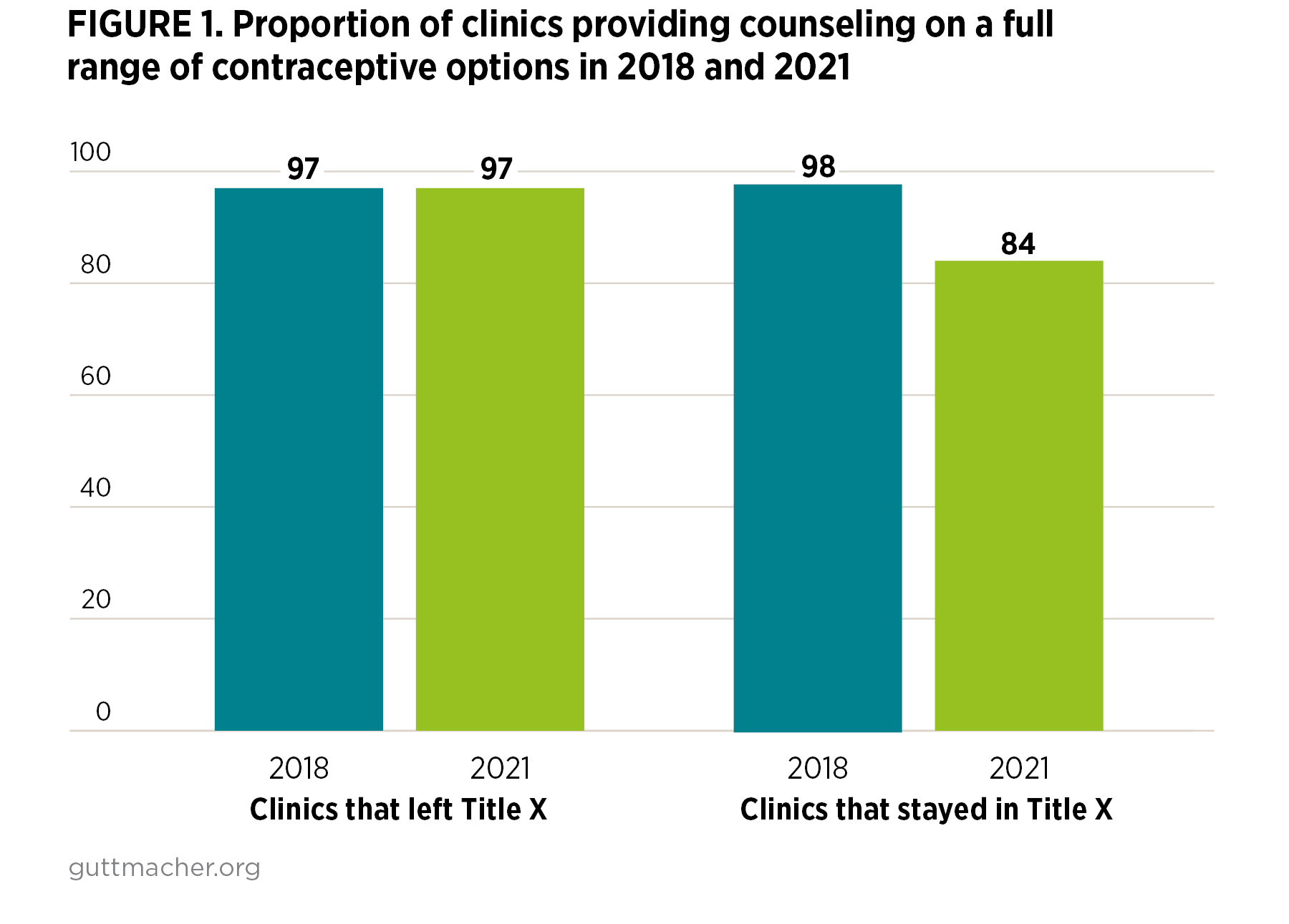
An RHIS study of family planning providers in Arizona, Iowa and Wisconsin shows that while the sites that remained in the Title X program and those that left following implementation of the Title X rule faced different challenges, both were impacted in ways that compromised their services and provision of person-centered care. For example, counseling on the full range of contraceptive methods declined among clinics that stayed in the Title X program from 98% to 84% (Figure 1), while most clinics that left the program continued to offer comprehensive contraceptive counseling (97%).13 Similarly, clinics that left the Title X program continued to offer a higher number of contraceptive methods than clinics that stayed in the program, with the gap widening after implementation of the rule (9.4 vs. 8.7 in 2018 and 9.6 vs 8.2 in 2021). Over the same period, nondirective pregnancy options counseling declined at sites that left the Title X program. While clinics that left Title X were not required to comply with the 2019 Final Rule’s ban on counseling for abortion, this decline may indicate the chilling effect of the rule on counseling practices.
Providers at clinics that remained in the Title X program reported not being able to provide comprehensive options counseling to pregnant patients as a result of the rule’s prohibition on abortion counseling and referrals.14 They stopped discussing abortion procedures, referring for abortion care or even offering a list of abortion providers. Some Title X providers reported fear of saying the wrong thing and not being able to provide patients with all the information relevant to their health. When providers cannot give their patients comprehensive information, communication, informed consent and trust, all of which are essential to person-centered care, are undermined. Centering reproductive autonomy requires giving providers the resources and support they need to rely on their expertise and provide patients with high-quality care.
Meanwhile, clinics that left Title X because of the 2019 rule had to grapple with the loss of a major funding source and access to discounted contraceptive services, forcing many to adapt fee models and reimbursement plans, which created more financial obstacles for patients.14 These obstacles can force providers and patients to make care decisions that are not centered on a patient’s needs and values but on financial and other constraints. In some cases, cost barriers resulted in some patients using health insurance when they otherwise may have chosen not to, which can cause privacy concerns for patients who are not the policyholders. In others, this led to a decrease in patients selecting higher-cost contraceptive methods such as long-acting reversible contraception (LARCs), even if that would have been their preferred choice.
Both clinics that remained in Title X and those that left the network reported strains as a result of staff challenges. These challenges were spurred by the impact of the Title X rule and the COVID-19 pandemic, as the latter affected nearly all health care workers. However, clinics that left Title X were more likely to report losing staff and to report staff retention and morale as the most important challenges they faced in 2021.13
How Policies Impact Patients’ Reproductive Autonomy and Person-Centered Care
Restrictions on reproductive health care systems and providers trickle down to impact individuals’ access to care and reproductive autonomy, which cannot be achieved unless providers are able to center patient needs in the provision of care. RHIS documented associations between policy changes and patients’ contraceptive outcomes—and examined patients’ preferences and whether they were met. Findings show that patients in Iowa who had accessed sexual and reproductive health care prior to the Final Rule at a Title X–funded health care center that subsequently left the network were less likely to have received recent contraceptive care after the rule was implemented, compared with those who had initially accessed this care at a site that either stayed in the network or was never a part of it.15 Further, these data, limited to the pre–COVID-19 time period, show that respondents in the first group were less likely to have been using a provider-involved method, less likely to have been using a method that carries a cost and less likely to report being satisfied with their method after the rule went into effect.
RHIS also identified barriers associated with cost, access and quality of care for patients in Iowa who were accessing contraception following a 2017 state policy change in which health care sites that provided abortion care or referrals were removed from the state’s Medicaid family planning program, the 2019 Title X Final Rule was implemented and the COVID-19 pandemic was just beginning.16 Taken together, these findings indicate that diminished access to high-quality, more affordable and more comprehensive sexual and reproductive health care may have resulted in patients shifting their contraceptive use to a method that they preferred less; such a reduction in individuals’ decision-making power runs counter to the tenets of reproductive autonomy.
These findings were not unexpected, given that care within the Title X network has been historically documented as being of high quality and centering patients’ needs and preferences.17,18 When policies undermine that network or the provision of care, they end up undermining person-centered care, the provider-patient relationship and patient health outcomes. When they are not faced with medically unnecessary restrictions, specialized reproductive health clinics are more likely to provide services that make initiating and continuing contraceptive use easier for patients, including providing prescriptions and refills for the pill on-site, avoiding unnecessary physical exams and offering same-day LARC insertions.19 Patients who rate their interpersonal interactions with their sexual and reproductive health care provider more favorably are more likely to still be using their contraceptive method after six months and to use more effective methods.20 Further, RHIS research of people seeking publicly funded family planning care in Arizona, Iowa and Wisconsin revealed that those who reported receiving person-centered contraceptive care had higher adjusted odds of being satisfied with their contraceptive method compared with those who did not receive person-centered care, but this association was only found among White patients.21
Recommendations
Policymakers must strive for sexual and reproductive health equity. Systemic racism, sexism and economic injustice have impacted sexual and reproductive health outcomes for too long.22–24 RHIS data show that policy restrictions on sexual and reproductive health care compound and further entrench these inequities. Instead, we need policies that promote meaningful access to care, the provision of person-centered care and reproductive autonomy. To help address the harmful impact of the 2019 Title X Rule, as well as other restrictive policies and the COVID-19 pandemic, and to build toward sexual and reproductive health equity in contraceptive access across the country, policymakers must take several steps.25
Fully fund and strengthen Title X. RHIS findings make clear that the Title X program must be both protected from political interference and strengthened. The Biden administration rolled back the 2019 Final Rule, but this is only the first step in ensuring that the program can fulfill its original mission to address systemic inequities in access to contraception and other sexual and reproductive health care services. In addition to facing politically motivated policies and challenges with staff morale, the Title X program has suffered chronic underfunding, making it impossible for it to meet the need for publicly funded sexual and reproductive health care across the country. While it is estimated that the Title X program would need annual appropriations of $737 million to serve all women in need of Title X services, the program has received only $286 million annually since the Centers for Disease Control and Prevention and Office of Population Affairs calculated that figure in 2016.26 Essentially, actual funding has decreased over time as a result of inflation.
Congress must take steps to ensure adequate funding for the program every year in the annual appropriations bill. In addition, lawmakers should ensure that Title X regulations and the underlying statute promote comprehensive, medically sound and patient-centered care, and are not subject to political intervention by any future administration aiming to undermine sexual and reproductive health and rights. Congress should codify provider nondiscrimination provisions in the Title X statute to ensure providers are not punished for providing, counseling about or referring for abortion.27
Ensure sexual and reproductive health care programs provide person-centered care. As is evident from the RHIS findings, restrictions on sexual and reproductive health care impose barriers that can make person-centered care impossible, even in programs intended to expand sexual and reproductive health care access. This was certainly true of the 2019 Title X rule—which targeted information about and referrals to abortion care, but had a sizable impact on the provision of contraceptive care. Not only must policymakers defend against such a gag rule ever being in place again, they must proactively ensure that new and existing programs that provide or increase access to reproductive health care do so in ways that support reproductive autonomy.
At a minimum, this means providers must be able to give patients full information about their care and possible options, including all forms of contraception and referrals to abortion care, without restrictions. All health plans and programs, including publicly funded health programs like Medicaid, must not only cover this person-centered counseling on comprehensive sexual and reproductive health care, but must also cover all contraceptive methods and abortion care.
Remove restrictions that silo abortion care. All forms of reproductive health care are inextricably linked. The harmful impact of the 2019 Title X Final Rule, as evidenced throughout the RHIS, clearly illustrates abortion stigma impacting other forms of sexual and reproductive health care. The extremes of the Title X Final Rule are not unique. Abortion care is often siloed from other forms of health care.28 In addition, anti-abortion stigma and restrictions not only impact access to abortion care but to all other forms of reproductive health care. As a result, policymakers must address these restrictions. This includes ending the Hyde Amendment, which prevents federal funds from covering abortion services for people enrolled in Medicaid, Medicare and the Children’s Health Insurance Program, and allowing social-safety-net sexual and reproductive health care providers, including federally qualified health centers and Title X providers, to support and provide patients with abortion counseling and services.
Require all health insurance plans and programs to provide comprehensive coverage for all contraceptive options. Baseline data collected in the RHIS confirm that cost is one of the most commonly cited barriers for individuals seeking reproductive health care. Nearly 20% of respondents in Arizona, Iowa and Wisconsin reported they had trouble or delays in obtaining their preferred method of birth control in the previous year, primarily as a result of cost and insurance-related barriers.29 While the 2019 Final Rule did not directly impose additional costs for contraceptive care on providers or patients, the rule’s restrictions caused funding shortfalls for many providers, which in some cases were passed onto patients. This impacted contraceptive outcomes for many patients, including a decrease in the use of provider-involved methods and patient satisfaction with the methods they choose.
Federal and state policies must require that all health plans and programs address cost issues by covering the full range of contraceptive options, including over-the-counter choices, without limitations, particularly for individuals enrolled in publicly supported health programs like Medicaid. This includes enforcing the Affordable Care Act’s (ACA) contraceptive coverage requirement and ensuring that all health plans and programs—including employer-based plans not subject to the requirement, Medicaid and Medicare—meet the ACA’s standard of ensuring access to all methods without cost sharing.
Ensure patients have multiple options for accessing reproductive health care. RHIS findings highlight the importance of ensuring a diversity of options that people can use to access reproductive health care. In Arizona, New Jersey and Wisconsin, despite different state contexts, women of reproductive age report similar levels of preferences for a wide range of sources to obtain contraception.30 These preferences range from accessing contraception by interacting with a health care provider in person to accessing contraception at a pharmacy—including over-the-counter methods—to receiving contraceptives via telehealth. The diversity of preferences makes clear that meaningful access looks different for different people and in different contexts.
To guarantee that individuals get the care they need in the way they prefer, public and private insurance programs should recognize and promote different options for accessing reproductive care at no cost. To do so, policymakers should increase access to high-quality telehealth care, including by insuring adequate reimbursement rates for telehealth in Medicare and Medicaid. In addition, policymakers should pass policies that would allow patients to access contraceptive care from the provider of their choice, including at the pharmacy or through the mail, increase access to over-the-counter contraceptives, and allow providers to dispense up to 12 months of contraception at a time and ensure that this prescription length is covered by health insurance plans.
Conclusion
The Reproductive Health Impact Study details the devastating impact of the overlapping crises of the Trump Title X Final Rule and the COVID-19 pandemic, but it also illustrates the intersectional impact of restrictions on reproductive health care. The case studies in Arizona, Iowa, New Jersey and Wisconsin make clear that these restrictions negatively impact the provision of care, the availability of patient-centered services and reproductive autonomy. Policy solutions that center and promote sexual and reproductive health equity are necessary to reverse the damage and address the crisis in reproductive health care across the country.
References
1. Neuman T et al., President Trump’s record on health care, KFF, 2020, https://www.kff.org/report-section/president-trumps-record-on-health-care-issue-brief.
2. Ross L and Solinger R, Reproductive Justice: An Introduction, Oakland: University of California Press, 2017.
3. Carrión F, Honoring reproductive justice founders during Black History Month, National Health Law Program, 2022, https://healthlaw.org/honoring-reproductive-justice-founders-during-black-history-month.
4. Bixby Center for Global Reproductive Health, Measuring women’s reproductive autonomy, San Francisco: University of California, San Francisco, 2014, https://bixbycenter.ucsf.edu/news/measuring-women%E2%80%99s-reproductive-autonomy.
5. Upadhyay UD et al., Development and validation of a reproductive autonomy scale, Studies in Family Planning, 2014, 45(1):19–41, doi:10.1111/j.1728-4465.2014.00374.x.
6. Institute of Medicine, Crossing the Quality Chasm: A New Health System for the 21st Century, Washington, DC: National Academy Press, 2001.
7. Hart J, Crear-Perry J and Stern L, US sexual and reproductive health policy: which frameworks are needed now, and next steps forward, American Journal of Public Health, 2022, (112):S518–S522, doi:https://doi.org/10.2105/AJPH.2022.306929.
8. Fowler CI, Gable J and Lasater B, Family Planning Annual Report: 2020 National Summary, Washington, DC: Office of Population Affairs, US Department of Health and Human Services, 2021, https://opa.hhs.gov/sites/default/files/2021-09/title-x-fpar-2020-national-summary-sep-2021.pdf.
9. Dawson R, Trump Administration’s Domestic Gag Rule Has Slashed the Title X Network’s Capacity by Half, New York: Guttmacher Institute, 2020, https://www.guttmacher.org/article/2020/02/trump-administrations-domestic-gag-rule-has-slashed-title-x-networks-capacity-half.
10. Office of Population Affairs, 50 years of Title X: a timeline of key events, Washington, DC: Department of Health and Human Services, 2020, https://opa.hhs.gov/sites/default/files/2020-11/opa-titlex-2020-timeline.pdf.
11. US Census Bureau, QuickFacts: United States, 2023, https://www.census.gov/quickfacts/fact/table/US/PST045223.
12. Marcella JS, The Title X program: setting standards for contraceptive and health equity, American Journal of Public Health, 2022, 112(S5):S511–S514, doi:10.2105/AJPH.2022.306900.
13. VandeVusse A et al., Publicly Funded Clinics Providing Contraceptive Services in Four US States: The Disruptions of the “Domestic Gag Rule” and COVID-19, New York: Guttmacher Institute, 2023, https://www.guttmacher.org/report/clinics-providing-services-in-four-us-states-disruptions-of-gag-rule-and-covid-19.
14. VandeVusse A et al., The impact of policy changes from the perspective of providers of family planning care in the US: results from a qualitative study, Sexual and Reproductive Health Matters, 2022, 30(1):2089322, doi:10.1080/26410397.2022.2089322.
15. Kavanaugh ML, Leong E and Haas M, Measuring the relationship between the 2019 Title X Final Rule and patients’ sexual and reproductive health care access and behavior in Iowa using a difference-in-difference approach, Sexuality Research and Social Policy, 2023, https://link.springer.com/article/10.1007/s13178-023-00876-2.
16. Frohwirth L et al., Access to preferred contraceptive strategies in Iowa: a longitudinal qualitative study of effects of shifts in policy and healthcare contexts, Journal of Health Care for the Poor and Underserved, 2022, 33(3):1494–1518, 10.1353/hpu.2022.0126.
17. Frost JJ et al., Variation in Service Delivery Practices Among Clinics Providing Publicly Funded Family Planning Services in 2010, New York: Guttmacher Institute, 2012, https://www.guttmacher.org/report/variation-service-delivery-practices-among-clinics-providing-publicly-funded-family-planning.
18. Wood S et al., Scope of family planning services available in federally qualified health centers, Contraception, 2014, 89(2):85–90, 10.1016/j.contraception.2013.09.015.
19. Zolna MR and Frost JJ, Publicly Funded Family Planning Clinics in 2015: Patterns and Trends in Service Delivery Practices and Protocols, New York: Guttmacher Institute, 2016, https://www.guttmacher.org/report/publicly-funded-family-planning-clinic-survey-2015.
20. Dehlendorf C et al., Association of the quality of interpersonal care during family planning counseling with contraceptive use, American Journal of Obstetrics and Gynecology, 2016, 215(1):78.e1–78.e9, 10.1016/j.ajog.2016.01.173.
21. Kavanaugh ML, Haas M and Douglas-Hall A, Differential associations between experiences of contraceptive care and subsequent contraceptive access and preferences among family planning patients by racial identity: evidence from Arizona, Iowa, and Wisconsin, currently under review.
22. Paradies Y et al., Racism as a determinant of health: A systematic review and meta-analysis, PLOS ONE, 2015, 10(9):e0138511, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4580597/.
23. Homan P, Sexism and health: advancing knowledge through structural and intersectional approaches, American Journal of Public Health, 2021, 111(10):1725–1727, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8561209/.
24. Cui X and Chang C-T, How income influences health: decomposition based on absolute income and relative income effects, International Journal of Environmental Research and Public Health, 2021, 18(20), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8535401/.
25. Planned Parenthood, New blueprint for sexual and reproductive health, rights, and justice policy agenda highlights specific actions for the executive branch, news release, Oct. 25, 2023, https://www.plannedparenthoodaction.org/pressroom/new-blueprint-for-sexual-and-reproductive-health-rights-and-justice-policy-agenda-highlights-specific-actions-for-the-executive-branch.
26. August EM et al., Projecting the unmet need and costs for contraception services after the Affordable Care Act, American Journal of Public Health, 2016, 106(2):334–341, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4985850/.
27. Dawson R, What federal policymakers must do to restore and strengthen a Title X family planning program that serves all, Guttmacher Policy Review, vol. 24, 2021, https://www.guttmacher.org/gpr/2021/03/what-federal-policymakers-must-do-restore-and-strengthen-title-x-family-planning-program.
28. Jones RK, Kirstein M and Philbin J, Abortion incidence and service availability in the United States, 2020, Perspectives on Sexual and Reproductive Health, 2022, 54(4):128–141, https://www.guttmacher.org/article/2022/11/abortion-incidence-and-service-availability-united-states-2020.
29. Fuentes L et al., Primary and reproductive healthcare access and use among reproductive aged women and female family planning patients in 3 states, PLOS ONE, 2023, 18(5):e0285825, 10.1371/journal.pone.0285825.
30. Kavanaugh ML and Zolna MR, Where do reproductive-aged women want to get contraception? Journal of Women’s Health, 2023, 32(6):657–669, https://pubmed.ncbi.nlm.nih.gov/37099807/.
Suggested Citation
Easter R, Friedrich-Karnik A and Kavanaugh M, Any Restrictions on Reproductive Health Care Harm Reproductive Autonomy: Evidence from Four States, New York: Guttmacher Institute, 2024, https://www.guttmacher.org/report/any-restrictions-reproductive-health-….
Acknowledgments
The authors thank Kelly Baden, Emma Stoskopf-Ehrlich and Alicia VandeVusse for their review and feedback on this report, which was edited by Peter Ephross and Chris Olah. All are with the Guttmacher Institute.
This study was made possible by a grant to the Guttmacher Institute from an anonymous donor and by the William and Flora Hewlett Foundation. The findings and conclusions in this report are those of the authors and do not necessarily reflect the positions and policies of the donors. The funders had no role in study design, data collection, analysis, decision to publish or preparation of the report.