- The COVID-19 pandemic and its associated restrictions raised concerns that adolescents in Uganda may face barriers to receiving family planning commodities and services.
- Public and private service statistics data reveal that Uganda experienced smaller and shorter pandemic-related disruptions in adolescent access to sexual and reproductive health services than were initially anticipated.
- A temporary dip in service visits during April 2020 was followed by a return to previous levels and even an increase in family planning visits among adolescent women during the remainder of 2020.
- These results speak to the resilience of the health system, which continued to provide services, and the impact of actions by partners to support access to reproductive health supplies and services.
- The Ministry of Health and other stakeholders should take the following steps to ensure adolescents’ continued access to sexual and reproductive health services throughout the remainder of the pandemic:
- Document and foster the adaptions and processes that helped ensure continuity of services during the COVID-19 restrictions, so that similar measures may be adopted in future crises.
- Promote meaningful participation of young people in COVID-19 task forces, to ensure that relevant policies are gender-inclusive and respond to young people’s sexual and reproductive health needs.
- Classify contraceptive care as an essential service, integrate it with COVID-19 response interventions and ensure that it remains fully operational and open before, during and after any future lockdowns.
Access to Contraceptive Services Among Adolescents in Uganda During the COVID-19 Pandemic

Author(s)
Fredrick Makumbi, Simon Peter Sebina Kibira, Lilian Giibwa, Chelsea Polis, Margaret Giorgio, Patrick Segawa, Lillibet Namakula and Ricardo MimbelaReproductive rights are under attack. Will you help us fight back with facts?
Key Points
Introduction
Uganda has one of the youngest populations in the world, with 78% of people younger than 30 and half younger than 15.1,2 This means that over the coming years, a growing proportion of the population will be sexually active and of reproductive age. The Ugandan government is committed to scaling up the use of modern family planning methods, to ensure that every woman in Uganda can choose when to have children and how many to have. Despite the tremendous efforts made by the government in the health sector, the need for sexual and reproductive health services, including those related to HIV, continues to rise.3,4 Further, the growing population of young people in Uganda and the associated increased demand for sexual and reproductive health services could outstrip the ability of policies and programs to meet these needs, placing an additional strain on the provision of sexual and reproductive health services.
The onset of the COVID-19 pandemic threatened to create additional barriers for adolescents wishing to access sexual and reproductive health services. Following the first reported case of COVID-19 in Uganda on March 21, 2020, the Ugandan government instituted a range of public health measures to restrict gatherings, in-school education, transportation and more.5 Lockdowns were implemented in a phased manner, starting with the closure of schools and other academic institutions. As the numbers of COVID-19 cases rose, new partial lockdown measures were put into place, such as a ban on the use of public transport (including taxis). Eventually, a 14-day lockdown was implemented on March 30, 2020, including a ban on private transport and a nationwide nighttime curfew. The lockdown was subsequently extended to May 5, 2020. Pandemic-related restrictions made it difficult for both workers and patients to reach health facilities. Fear of being at a health facility was widespread, and many believed these to be either closed or restricted to COVID care and treatment. Community health workers, who play an important role in health promotion, referrals and community health outreach in Uganda, often paused their usual activities during the lockdown.6
The overwhelming burdens placed on health facilities during the COVID-19 pandemic have raised concerns about its impact on women’s ability to access family planning supplies and services. To counteract these challenges, the Ugandan government, in collaboration with development and implementing partners, worked to protect pregnant women’s access to maternity services and more general access to essential sexual and reproductive health information and services, such as condoms and other contraceptives, comprehensive sexuality education, obstetric care, menstrual health materials, counseling and gender-based violence support.7 Among other steps, the government recruited more than 200 additional health workers, to reduce pressure on the existing health workers; ensured continued provision of routine and emergency health services, including family planning, immunization and delivery care; printed and distributed nationwide COVID-specific informational materials in local languages; and issued special travel permits to patients and health care workers across the country.8 Development partners engaged key stakeholders (e.g., opinion leaders, champions, trendsetters and young people) in health promotion; worked to continue providing important health services (especially youth-friendly services) throughout the lockdown; utilized existing community-level structures to extend service delivery and information to people throughout the country; and provided the government with advice on how to mitigate the lockdown’s impact on access to community health services.
Despite these concentrated efforts, concerns remain about the potential impact of the COVID-19 pandemic on adolescent health care in Uganda; this report compiles data from several sources to shed light on that impact. The results of this report suggest that despite some concentrated declines during the initial lockdown months, Uganda was able to maintain or restore access to essential health services, including family planning. We provide evidence that the country experienced smaller and shorter disruptions in access to sexual and reproductive health services than initially anticipated. This evidence highlights a temporary dip in family planning use among Ugandan women aged 15–19 during April and May 2020 related to COVID-19 restrictions, followed by sustained increases over the remainder of 2020. This speaks to the resilience of Uganda’s health systems, which continued to provide services, and the impact of actions by partners to support access to reproductive health supplies and services.
Methods
A detailed description of the data sources and analytic techniques used in this report and some supplementary analyses are provided in the Data and Methods Appendix (download above). In brief, two private nongovernmental organizations, which we refer to here as Private Provider #1 and Private Provider #2, furnished service delivery data for the geographic areas of Uganda that they served in 2019 and 2020. For Private Provider #1, we compared their internal projections for caseloads from March to November 2020 to the number of actual client visits during that time frame. For Private Provider #2, we compared levels of service provision from March to December 2019 with those of March to December 2020. In addition, we used national-level service delivery data for the period 2018–2020 from Uganda’s Health Management Information System (HMIS) to examine trends in adolescents’ use of public sexual and reproductive health services before and during the pandemic. Finally, to understand overall trends in modern contraceptive use among adolescent women, we abstracted data from nationally representative, population-based surveys conducted by Performance Monitoring for Action Uganda.9
Adolescents’ Use of Modern Contraceptive Services
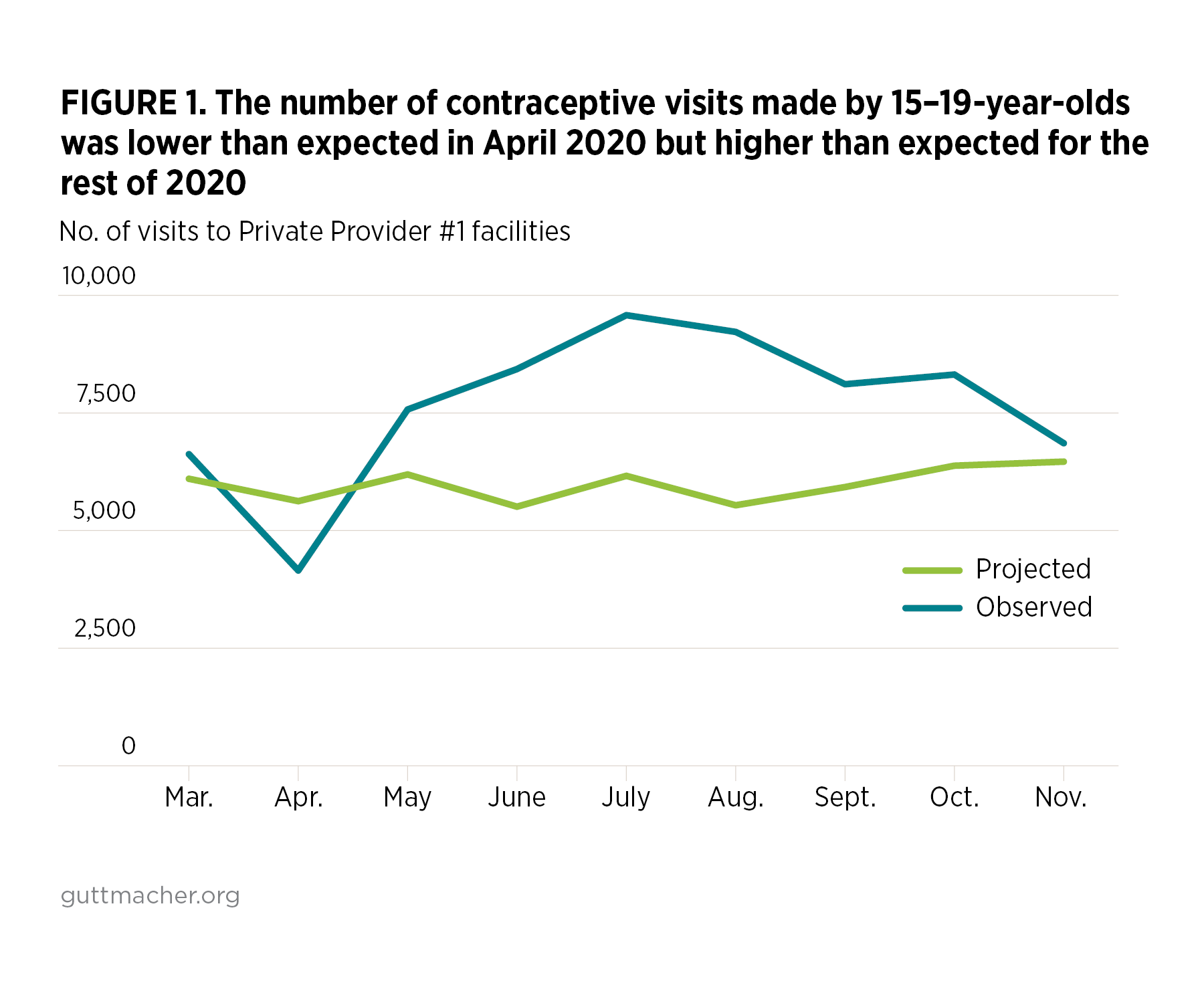
Data from Private Provider #1 show an initial decrease in adolescent contraceptive visits at the start of the pandemic; actual visits dipped far below the number projected by the provider for April 2020 (Figure 1). However, adolescents’ visits for contraceptive services rebounded starting in May 2020 and continued to exceed projections through November 2020.
Data from Private Provider #2 tell a slightly more nuanced story. Overall, modern contraceptive visits among adolescent women aged 15–19 were lower in every month of 2020 than in the same month in 2019. However, this overall trend masked important differences by type of family planning method. The sustained decrease seen in all contraceptive visits seems to have been driven largely by visits for internal and external condoms (i.e., female and male condoms). This makes sense, given that Private Provider #2 closed a program in March 2020 that included peer distribution of condoms to young people in communities and learning institutions.
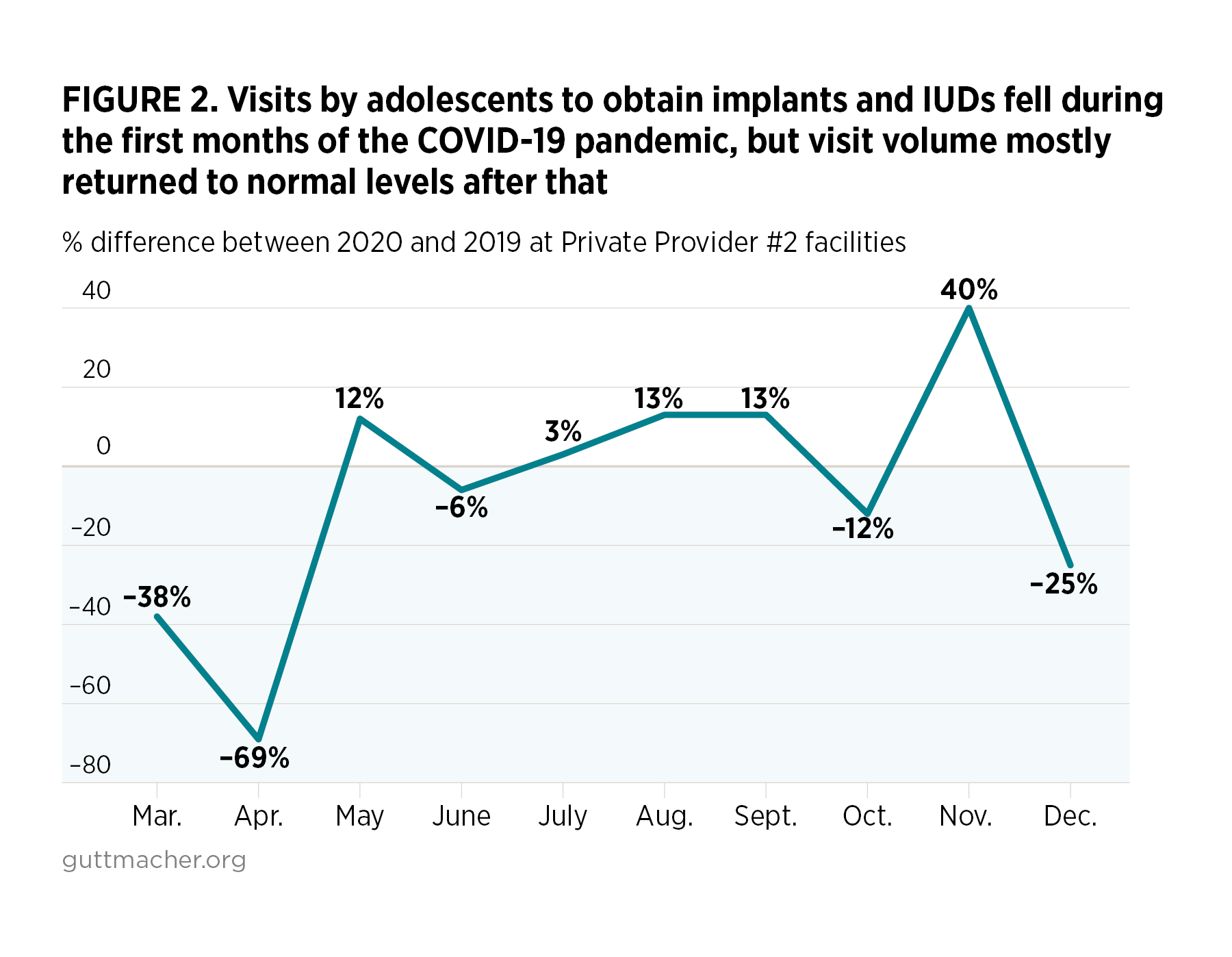
On the other hand, visits for other contraceptive methods followed a pattern similar to what was seen for Private Provider #1. For example, compared with March and April 2019, substantial declines in visits for IUDs and implants were observed in March 2020 (a decrease of 38%) and April 2020 (a decrease of 69%; Figure 2). Thereafter, however, visits for IUDs and implants returned to being roughly at or above 2019 levels for most of remainder of 2020. Similar patterns can be seen for pills and injectables.
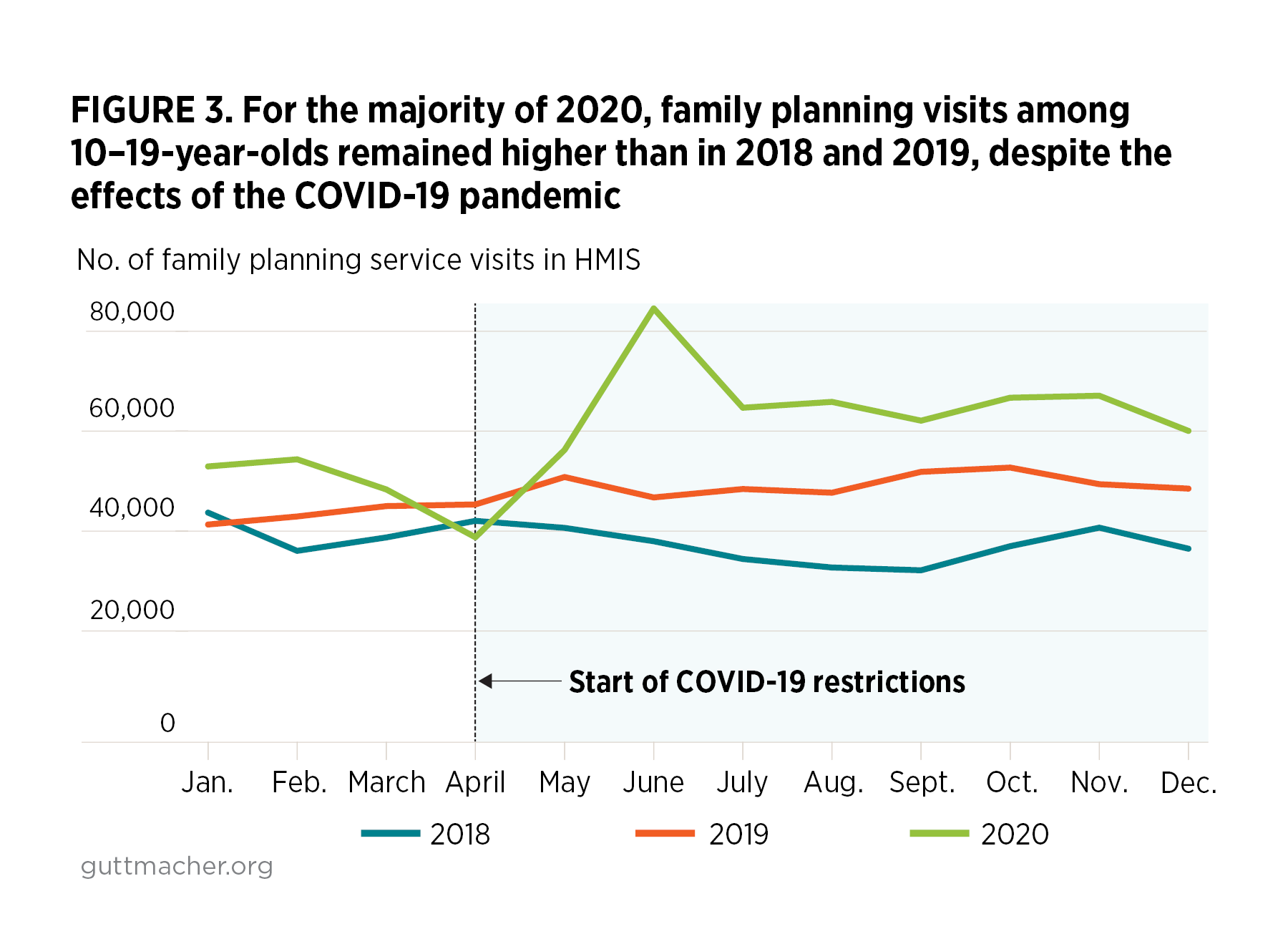
HMIS data show that family planning service visits among 10–19-year-olds increased between 2018 and 2019 across all calendar months except January (Figure 3). However, in line with the trend seen for the two private providers, service visits declined at the start of the COVID-19 lockdown in April 2020 to a level lower than in the corresponding months of 2018 and 2019. The rebound from this drop was swift, and over the next months, the HMIS data show family planning service visits rising to levels above those observed for 2018 and 2019. On average, adolescent family planning service visits were consistently higher in 2020 than in 2019 across all months except for April 2020, when visits were 15% lower than in April 2019.
The modern contraceptive prevalence rate among adolescents aged 15–19 increased by 3.6 percentage points—or 37%—between the April 2019 (10%) and September 2020 (13%) Performance Monitoring for Action surveys. Several characteristics were associated with a statistically significant increase in the modern contraceptive prevalence rate between the two surveys. For example, modern contraceptive prevalence rate among adolescents aged 18–19 was 58% higher in the 2020 survey than in the 2019 survey. Likewise, prevalence rates were higher in 2020 than in 2019 for 15–19-year-olds who were married or in a union (68%), who had completed primary schooling (64%), who were sexually active (81%), who lived in a rural area (43%), who were in the second-poorest wealth quintile (159%) and who were exposed to family planning messages (33%).
Adolescents’ Use of Postabortion Care Services
Data on postabortion care were available only from Private Provider #2. In total, the number of postabortion care patients served by this provider increased by 34%, on average, between March and December 2020, compared with the same months in 2019. There are several possible explanations for this increase, including an increase in unintended pregnancy and abortion in Uganda during the COVID-19 pandemic. However, it is difficult to know for certain what may have driven this change in caseloads.
Conclusions and Recommendations
Overall, the data presented in this report show the COVID-19 pandemic to have had minimal to no effect on adolescents’ access to family planning services in Uganda. HMIS data and those from private providers suggest a dip in access to some family planning services during April 2020, when a total lockdown was enforced. The Performance Monitoring for Action survey data show an increase in contraceptive use among 15–19-year-olds between 2019 and 2020, which is in line with service data from the HMIS. The limited postabortion care data show that more adolescents sought care in 2020 than in 2019, which may reflect an increase in abortion cases.
The findings described here should be interpreted with some limitations in mind. Data from the HMIS are routine service data, reflecting a month-by-month picture of service visits at reporting facilities. The system does not capture data on those who receive services from nonreporting facilities. The Performance Monitoring for Action data are nationally representative cross-sectional sample surveys and only show current contraceptive method use at two points in time (April 2019 and September 2020). The rise in the modern contraceptive prevalence rate may have occurred prior to COVID-19 or after restrictions were imposed. A drop-off during the lockdown period may not be easily accounted for in these surveys, as the second survey was carried out after restrictions had been lifted in May 2020.
Based on these findings, Uganda’s Ministry of Health and private health providers could take several steps to ensure that adolescents continue to have access to sexual and reproductive health services throughout the remainder of the COVID-19 pandemic:
- Increasing the use of community health workers can reduce the burden on staff at health facilities and may increase the promotion and uptake of preventive health behaviors. Close coordination between Uganda’s Ministry of Health, district-level governments, service providers, and advocates is vital to strengthening the health system by recruiting, training and supporting a network of community health workers to deliver essential, high-quality services.
- The adaptations and processes that helped ensure continuity of services during the COVID-19 restrictions need to be documented and fostered, so that similar measures may be adopted in any future crisis.
- The meaningful participation of young people in COVID-19 task forces should be promoted, to ensure that relevant COVID-19 policies are gender-inclusive and responsive to young people’s sexual and reproductive health needs. The apparent reduction in access to condoms and to long-acting contraceptives may warrant greater investment in the provision of both short-acting and long-acting methods, to enable young people’s access to a wide range of services.
- Contraceptive services should be classified as essential services to be integrated with the COVID-19 response interventions and should remain fully operational and open before, during and after the lockdown. Services must adhere to the Ministry of Health’s Standard Operating Procedures.
Advocacy efforts to promote sexual and reproductive health among adolescents should also work to ensure equitable access to contraceptive services, particularly for vulnerable and marginalized adolescent populations (such as adolescents with disabilities) through already accredited private health care facilities, clinics, pharmacies and drug shops within the communities. In addition, these advocacy activities should promote strengthening supply chain management, with a focus on the "last mile" delivery of family planning commodities and supplies, to ensure method continuation and access.
REFERENCES
1. International Youth Foundation (IYF), Navigating Challenges: Charting Hope. A Cross-Sector Situational Analysis on Youth in Uganda, Vol. 1: Main Report, Baltimore, MD, USA: IYF, 2011, http://www.youthpolicy.org/national/Uganda_2011_Youth_Mapping_Volume_1….
2. Uganda Bureau of Statistics (UBOS), National Population and Housing Census 2014—Main Report, Kampala, Uganda: UBOS, 2016, http://www.ubos.org/wp-content/uploads/publications/03_20182014_Nationa….
3. Sexual and Reproductive Health and Rights (SRHR) Alliance, Increasing Youth-Friendly Sexual and Reproductive Health Services, Utrecht, Netherlands: Rutgers International, 2016, https://rutgers.international/resources/increasing-youth-friendly-sexua….
4. United Nations Population Fund (UNFPA), Delivering an Integrated Package of Rights: Linking Sexual and Reproductive Health with HIV Prevention and Gender Based Violence Services, Kampala, Uganda: UNFPA, 2018, http://uganda.unfpa.org/sites/default/files/pub-pdf/Issue%20brief%209%2….
5. Uganda Ministry of Health, Coronavirus (pandemic)—Covid 19, no date, http://www.health.go.ug/covid/.
6. Waiswa P, Sexual Reproductive Health and COVID-19 in Uganda: Avoiding the Pitfalls of Unintended Consequences for Maternal, Newborn, Child, Adolescent, and Nutrition Health in the National Response, Technical Brief Series, Kampala, Uganda: JAS Programme, 2020, https://www.sexrightsafrica.net/wp-content/uploads/2020/05/COVID-19-AND….
7. How Covid-19 is affecting reproductive health efforts, Daily Monitor, April 24, 2020, http://www.monitor.co.ug/uganda/magazines/full-woman/how-covid-19-is-af….
8. Ministry of Health, Update on the COVID-19 Response in Uganda, press release, Kampala, Uganda: Ministry of Health, April 2, 2020, https://www.health.go.ug/covid/2020/04/02/update-on-the-covid-19-respon….
9. Performance Monitoring for Action, Uganda, 2021, www.pmadata.org/countries/uganda.
Suggested Citation
Makumbi F et al., Access to Contraceptive Services Among Adolescents in Uganda During the COVID-19 Pandemic, New York: Guttmacher Institute, 2021, https://www.guttmacher.org/report/impact-covid-19-on-adolescent-srh-uga….
Acknowledgments
This report was written by Fredrick Makumbi, Simon P.S. Kibira and Lilian Giibwa, all of the School of Public Health, College of Health Sciences, Makerere University, Kampala, Uganda; Chelsea B. Polis, Margaret Giorgio and Ricardo Mimbela, all of the Guttmacher Institute, New York; and Patrick Segawa and Lillibet Namakula, both of Public Health Ambassadors Uganda (PHAU), Kampala, Uganda. It was edited by Michael Klitsch, and the figures were designed by Michael Moran; both are of the Guttmacher Institute. The authors thank the Ugandan Ministry of Health, the Performance Monitoring for Action project and the two private health services providers for providing access to the data used in these analyses.
Additional Downloads
- Data and Methods Appendix adolescent-srh-uganda-data-methods-appendix.pdf
Topic
Global
Tags