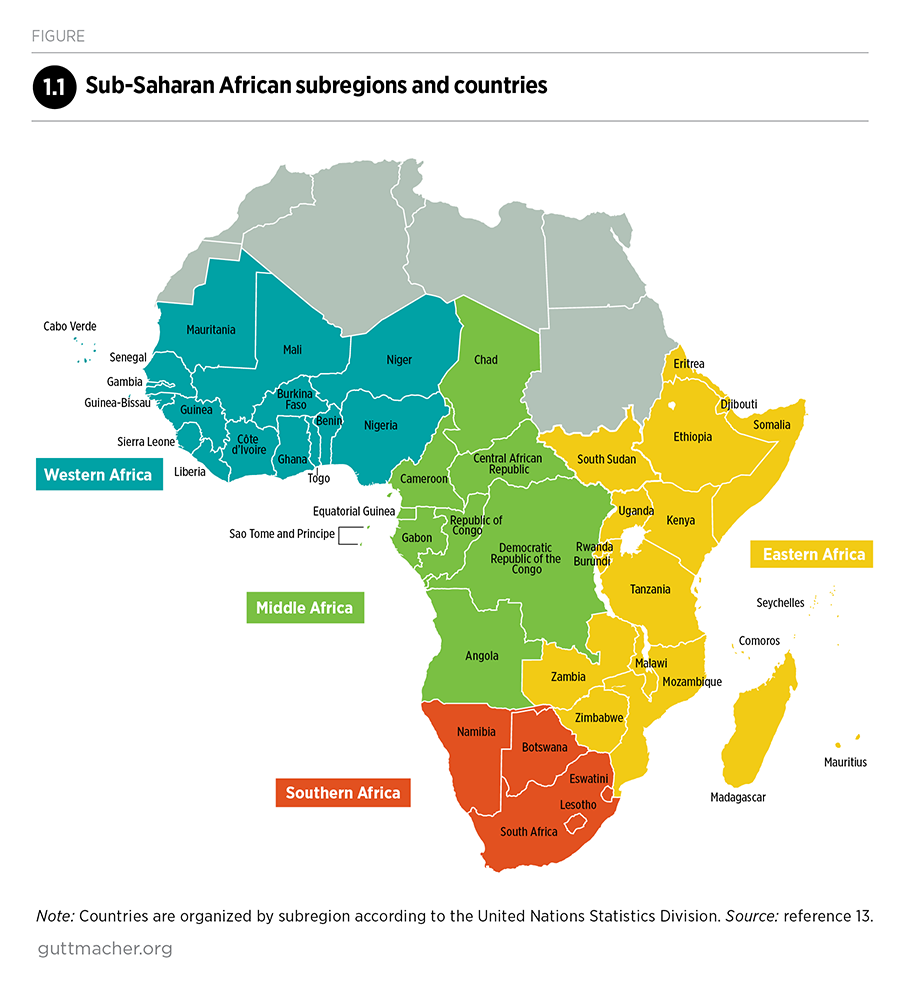
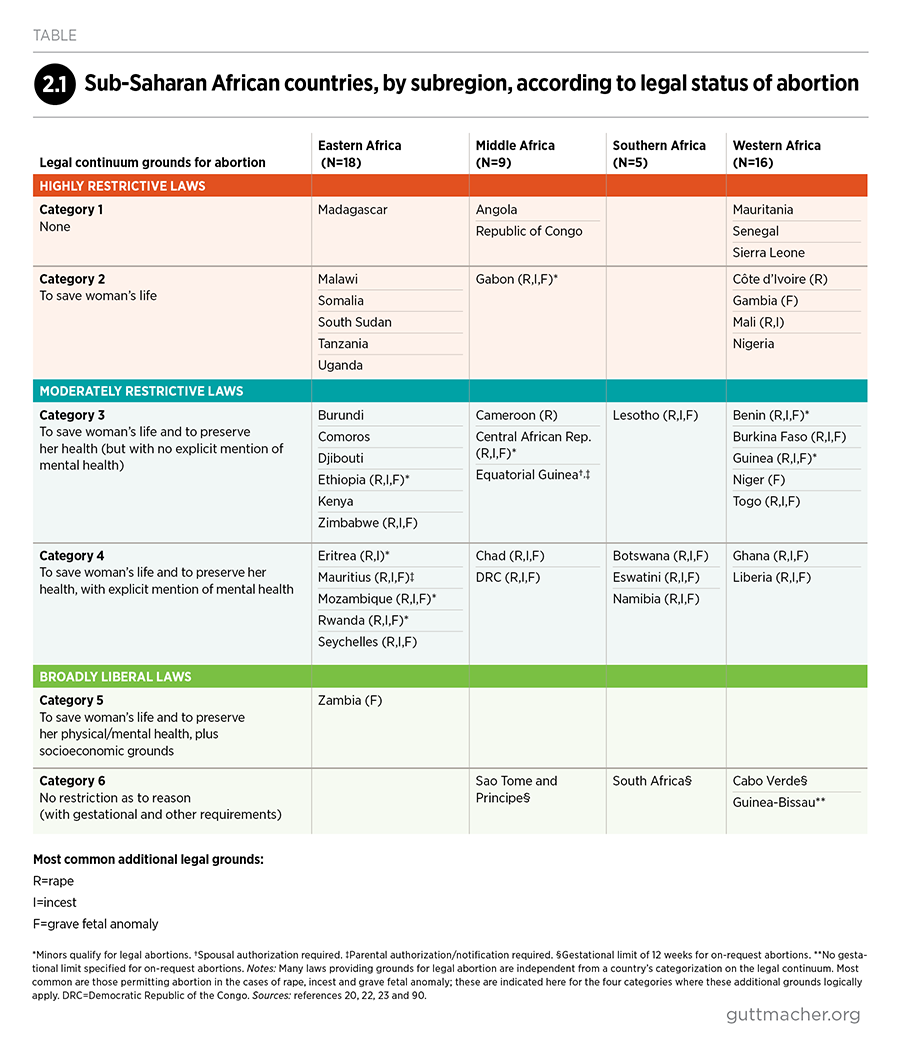
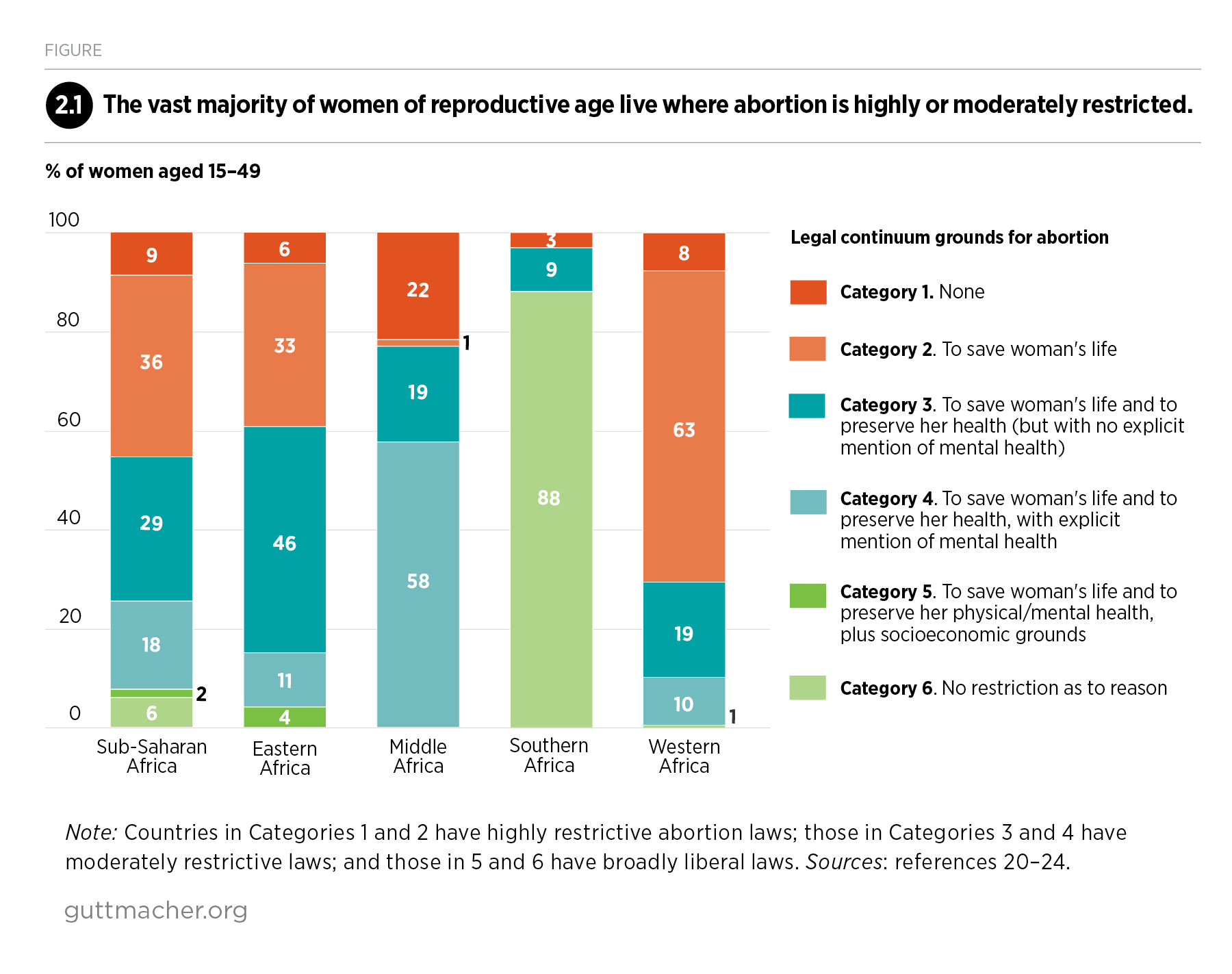
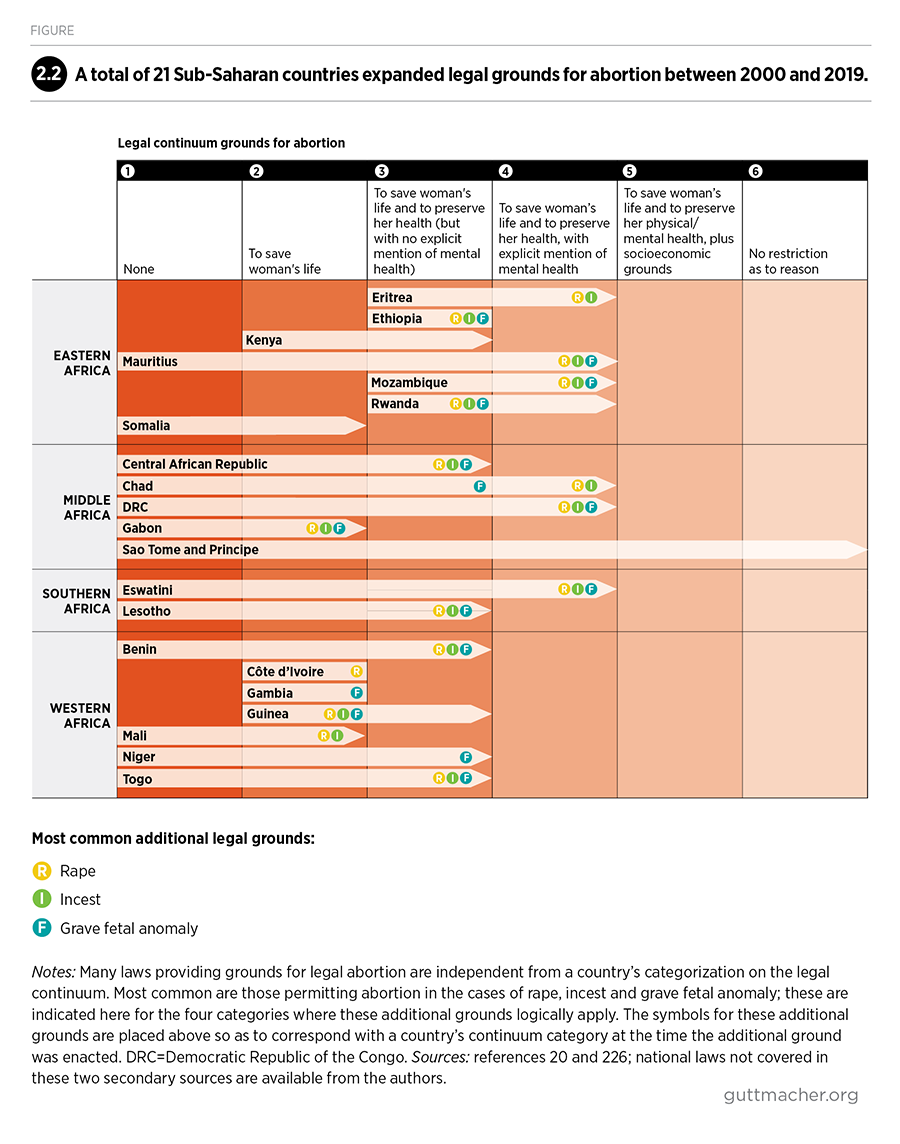
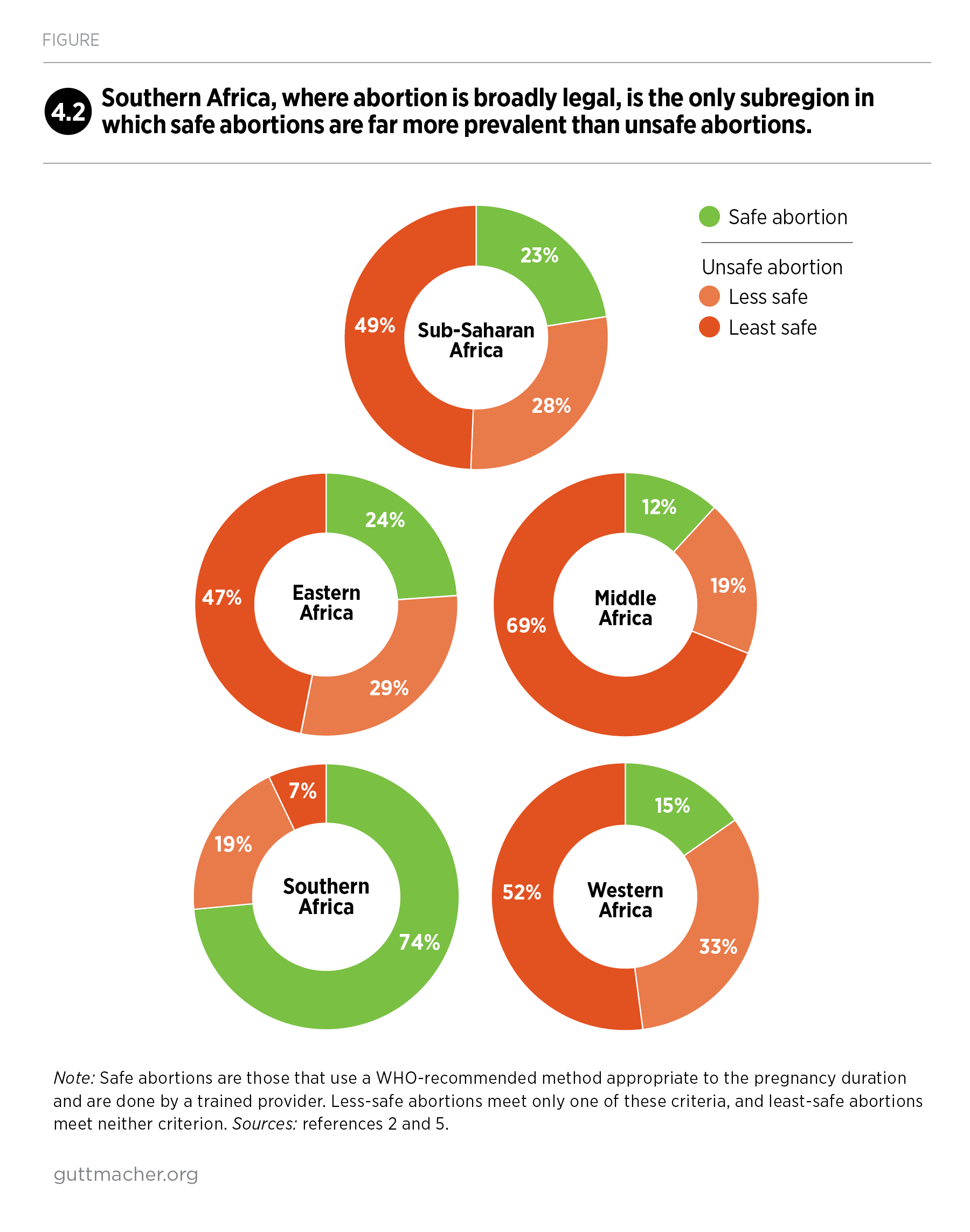
This report represents the first comprehensive compilation of information about abortion in Sub-Saharan Africa and its four subregions. It offers a panorama of this hard-to-measure practice by assembling data on the incidence and safety of abortion, the extent to which the region’s laws restrict abortion, and how these laws have changed between 2000 and 2019.
Many countries in this region have incrementally broadened the legal grounds for abortion, improved the safety of abortions, and increased the quality and reach of postabortion care. There is still much progress to be made, however, including enabling the region’s women to avoid unintended pregnancies and unsafe abortions. The report concludes with recommendations for a broad range of actors to improve the sexual and reproductive health and autonomy of the region’s 255 million women of reproductive age.